Trial of new stem cell therapy for dystrophic epidermolysis bullosa (RDEB) gives promising results
Posted: 1 June 2015 |
Results from a trial of a new stem-cell based therapy for a rare skin condition, recessive dystrophic epidermolysis bullosa (RDEB), have been published…
Promising results from a trial of a new stem-cell based therapy for a rare and debilitating skin condition, recessive dystrophic epidermolysis bullosa (RDEB), have been published.
RDEB is a painful skin disease in which very minor skin injury leads to blisters and poorly healing wounds. About 1,000 people in the UK live with RDEB. The fragile skin in RDEB also scars, develops contractures and is prone to life-shortening skin cancers. There is currently no cure for RDEB.
The therapy, involving infusions of stem cells, was found to provide pain relief and to reduce the severity of this skin condition for which no cure currently exists.
The clinical trial, led by King’s College London in collaboration with Great Ormond Street Hospital (GOSH), recruited 10 children with RDEB. The Phase I/II EBSTEM trial, funded by the Sohana Research Fund with donations from Goldman Sachs Gives, tested the safety of the treatment and also sought to establish whether it could help to reduce the severity of the disease and improve quality of life for these patients.
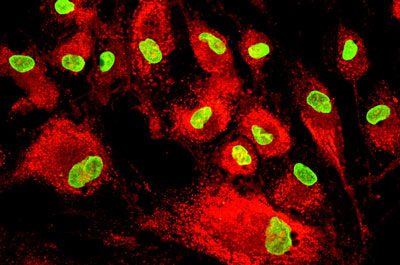
During the first six months of the trial, participants were given three infusions of mesenchymal stromal cells (stem cells) grown from the bone marrow of unrelated donors. Mesenchymal stem cells (MSCs) have been shown to home to wounded tissue and mediate wound healing in previous studies. Although the cells do not survive permanently, they may still deliver clinical benefits.
Severity of RDEB reported to have lessened following stem cell infusions
The children were then monitored for a year after the cell infusions. A range of monitoring tests showed no serious adverse effects in patients who received the therapy. The pain score (level of pain) reported was on average lower than before treatment, and the severity of the condition was also reported to have lessened following the infusions. Parents also reported better wound healing, less skin redness and fewer blisters.
Further work is needed to better understand the mechanisms involved – for example, whether the stem cells trigger the production of a variety of growth factors and cytokines – immune system regulators – to stimulate wound healing and reduce inflammation in the skin. Further studies are also needed to confirm the efficacy of the treatment and establish the optimal dose of cells to give RDEB patients.
Dr Gabriela Petrof, lead author from St John’s Institute of Dermatology at King’s College London, said, “We found that wound healing improved in all 10 children and the skin was less inflamed. Many of the kids also mentioned their skin was less painful and itchy, and their parents noted how much more energetic they were.”
Injecting MSCs raised no safety concerns
Professor John McGrath, senior author from St John’s Institute of Dermatology at King’s College London and honorary consultant dermatologist at Guy’s and St Thomas’ NHS Foundation Trust, added, “In 25 years of my research on RDEB, this is the only time I have seen any treatment change the nature of the condition. The outcomes are truly impressive and injecting the MSCs raised no safety concerns. At the same time, it’s important to note that this is not a cure and that the benefits wear off after about six months.
“Moving forward, we are now starting to introduce repeated infusions of MSCs into routine NHS clinical care. But we are also starting new clinical trials – combining cell and gene therapy to give patients with RDEB, children and adults, even better treatments as we search for a cure for this devastating inherited skin condition.”
Dr Anna Martinez, principal investigator from Great Ormond Street Hospital, said, “Giving the cells is straightforward, but we now have to fine tune the optimal dose and interval between infusions whilst work continues on more long term-therapies.”
The study was also supported by the UK National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London.
The results are published in in the Journal of Investigative Dermatology.
Related topics
Related organisations
King's College London, National Institute for Health Research (NIHR)




