FDA approves third gene therapy for large B-cell lymphoma
Posted: 8 February 2021 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
Breyanzi (lisocabtagene maraleucel) was approved on the 54 percent complete remission rate achieved in diffuse large B-cell lymphoma trials.
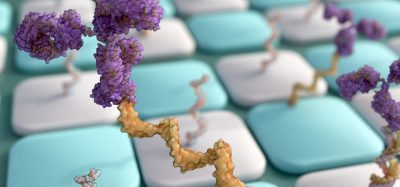
Breyanzi (lisocabtagene maraleucel), a chimeric antigen receptor (CAR) T cell-based gene therapy to treat adult patients with certain types of large B-cell lymphoma who have not responded to, or relapsed, after at least two other types of systemic treatment has been approved by the US Food and Drug Administration (FDA).
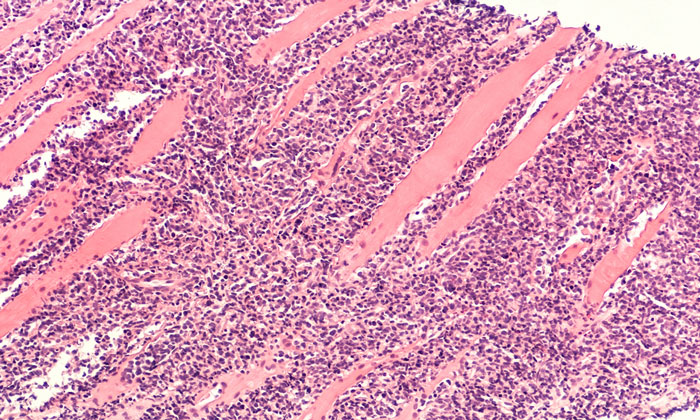
According to the agency, Breyanzi is the third gene therapy approved in the US for certain types of non-Hodgkin lymphoma, including diffuse large B-cell lymphoma (DLBCL). Breyanzi is not indicated for the treatment of patients with primary central nervous system lymphoma.
“Today’s approval represents another milestone in the rapidly progressing field of gene therapy by providing an additional treatment option for adults with certain types of cancer affecting the blood, bone marrow, and lymph nodes,” commented Dr Peter Marks, director of the FDA’s Center for Biologics Evaluation and Research. “Gene and cell therapies have evolved from promising concepts to practical cancer treatment regimens.”
DLBCL is the most common type of non-Hodgkin lymphoma in adults. Approximately 77,000 new cases of non-Hodgkin lymphoma are diagnosed in the US each year, with DLBCL accounting for around a third of newly diagnosed cases.
Breyanzi is customised for each patient; their T cells, a type of white blood cell, are collected and genetically modified to include a new gene that facilitates targeting and killing of the lymphoma cells. Once the cells are modified, they are infused back into the patient.
The safety and efficacy of the treatment were established in a multi-centre clinical trial of more than 250 adults with refractory or relapsed large B-cell lymphoma. The complete remission rate after treatment with Breyanzi was 54 percent.
The treatment can cause severe side effects, including cytokine release syndrome (CRS), which is a systemic response to the activation and proliferation of CAR T cells, causing high fever and flu-like symptoms and neurologic toxicities. Both CRS and neurological events can be life-threatening, so the therapy is being approved with a risk evaluation and mitigation strategy (REMS) which includes elements to assure safe use (ETASU).
The requirements include, among other things, that healthcare facilities that dispense Breyanzi be specially certified, with staff involved in the prescribing, dispensing or administering of the treatment being trained to recognise and manage the risks of CRS and neurologic toxicities.
Other side effects include hypersensitivity reactions, serious infections, low blood cell counts and a weakened immune system. According to the FDA, side effects generally appear within the first one to two weeks following treatment, but some side effects may occur later.
To further evaluate the long-term safety, the FDA is also requiring the manufacturer to conduct a post-marketing observational study involving patients treated with Breyanzi.
The approval was granted to Juno Therapeutics Inc., a Bristol-Myers Squibb Company.
Related topics
Anti-Cancer Therapeutics, Biologics, Clinical Trials, Drug Safety, Immunotherapy, Regulation & Legislation, t-cells
Related organisations
Juno Therapeutics Inc., US Food and Drug Administration (FDA)