Melflufen increases refractory multiple myeloma survival in Phase III study
Posted: 13 September 2021 | Anna Begley (European Pharmaceutical Review) | No comments yet
Melfufen met the primary endpoint of superior progression free survival (PFS) with a median of 6.8 months in Phase III OCEAN trial.
Oncopeptides AB presented data from the Phase III OCEAN study, a direct head to head comparison of the efficacy and safety of melflufen (melphalan flufenamide) plus dexamethasone and pomalidomide plus dexamethasone in patients with relapsed refractory multiple myeloma (RRMM), who are refractory to lenalidomide and have received two to four prior lines of therapy. The data was presented at the 18th International Myeloma Workshop (IMW) in Vienna.
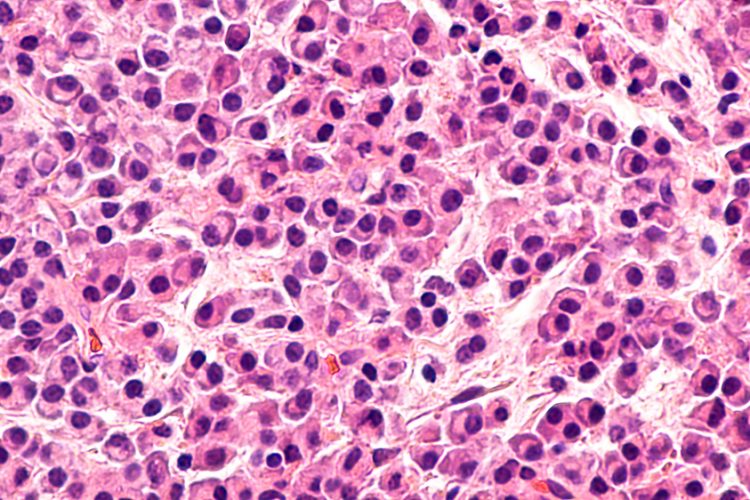
Melphalan flufenamide, also known as melflufen, is a first-in-class peptide-drug conjugate that targets aminopeptidases and rapidly releases alkylating agents inside cancer cells. Aminopeptidases are over-expressed in multiple myeloma cells and are associated with advanced disease and tumour mutational burden. According to Oncopeptides, targeting aminopeptidases causes selective activity in cancer cells, sparing healthy cells.
The Phase III OCEAN study was a global, randomised, head-to-head, open-label study, evaluating the efficacy and safety of melflufen and dexamethasone, versus pomalidomide and dexamethasone in patients with relapsed refractory multiple myeloma who have received two to four prior therapies.
Melflufen met the primary endpoint of superior Progression Free Survival (PFS) as assessed by the Independent Review Committee (IRC), with a median PFS of 6.8 months, compared to 4.9 months for pomalidomide, a Hazard Ratio (HR) of 0.79, and a p-value of 0.03. The results of key secondary endpoints in the Intention to Treat (ITT) population were Overall Survival (OS), which favoured pomalidomide with a HR of 1.10, and Overall Response Rate (ORR), where melflufen had a numerically higher ORR of 33 percent compared to 27 percent for pomalidomide.
An extensive analysis of data in pre-specified subgroups showed that the PFS benefit of melflufen mainly was driven by patients without a prior autologous stem cell transplant (ASCT), with a median PFS of 9.3 months versus 4.6 months and a HR of 0.59, compared to pomalidomide.
Furthermore, the OS data in patients with no prior ASCT favoured melflufen with a median OS of 21.6 months compared to 16.5 months for pomalidomide with a HR of 0.78. However, the OS results in patients with a prior autologous stem cell transplant favoured pomalidomide, with a median OS of 31.0 months versus 16.7 months for melflufen, and a HR of 1.61. This benefit of pomalidomide over melflufen in the ASCT subgroup has contributed to the HR of 1.1 in the ITT population.
Melflufen plus dexamethasone treatment resulted in substantially more grade 3/4 haematologic adverse events, when compared to pomalidomide. These were clinically manageable and in line with previous reports but more dose modifications were needed with melflufen when compared to pomalidomide.
“Results from the OCEAN study suggests that melflufen plus dexamethasone may become a potential treatment for patients with lenalidomide-refractory RRMM who have received two to four previous lines of therapy and who have not received a prior autologous stem cell transplant,” commented Fredrik Schjesvold, Head of Oslo Myeloma Center. “These patients represent a highly underserved population.”
Related topics
Anti-Cancer Therapeutics, Big Pharma, Clinical Trials, Data Analysis, Drug Safety, Research & Development (R&D), Therapeutics





![Roche logo sign lit up [Credit: testing/Shutterstock.com].](https://www.europeanpharmaceuticalreview.com/wp-content/uploads/Roche-3-400x187.jpg)



