Leveraging innate cell engagers for lymphoma treatment
Posted: 28 December 2023 | Caroline Peachey (European Pharmaceutical Review) | No comments yet
In this interview, Andreas Harstrick, CMO of Affimed discusses the evolution of the lymphoma treatment landscape and the promise of innate cell engagers for treating cancer.
In this exclusive interview, Andreas Harstrick, the Chief Medical Officer of Affimed unveils the potential of innate cell engagers for treating lymphoma. As well as presenting recent findings from the pivotal AFM13-104 study, Andreas also reflects on the challenges encountered and conquered in developing Affimed’s innate cell engager, Acimtamig, which targets CD30 on lymphoma cells and CD16A on NK cells.
Finally, Andreas looks at the prospects for antibodies that target the innate immune system in treating both haematological malignancies and solid tumours.
How has the treatment landscape for lymphoma evolved over the past few years?
When the patient’s lymphoma relapses after treatment with chemotherapy, BV and CPIs, there are no effective treatment alternatives”
Andreas Harstrick (AH): Over the last decade, the treatment paradigm particularly in Hodgkin lymphoma (HL) has significantly shifted with the introduction of brentuximab vedotin (BV) and checkpoint inhibitors (CPIs). Following their introduction, these therapies have moved to early lines of treatment, but unfortunately, a significant number of patients are not cured with these approaches. As a result, when the patient’s lymphoma relapses after treatment with chemotherapy, BV and CPIs, there are no effective treatment alternatives for these patients.
The situation is even more dire for patients with Peripheral T-cell lymphoma (PTCL), the population we will be focusing on next (eg, adding an exploratory PTCL cohort to LuminICE-203).
Why does AFM13 in combination with cord blood-derived natural killer (cbNK) have potential as treatment for this disease?
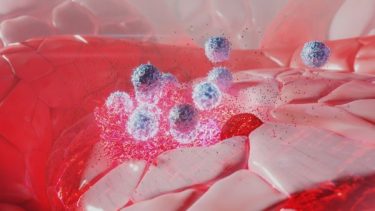
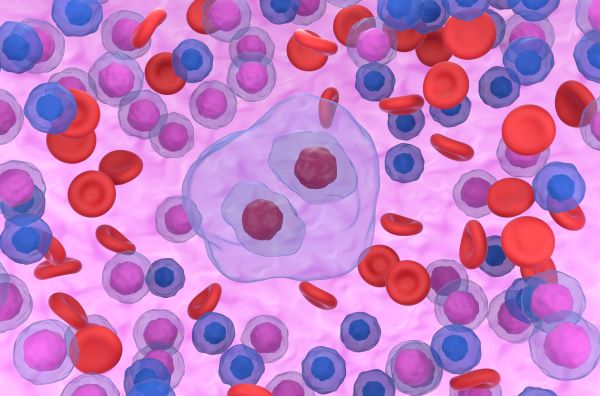
Illustration showing NK cells attacking tumour cancer cells
AH: Acimtamig, Affimed’s first-in-class innate cell engager (ICE®) targets CD30 on lymphoma cells and CD16A on NK cells. NK cells are the first line of defence in our body and our approach helps these cells to better detect and destroy the tumour. Many cancer patients, however, lack a functional innate immune system, and do not have enough functional NK cells. That is why we see that combining our ICE molecules with allogeneic NK cells can provide added benefit for the patient.
We have established a solid clinical proof of concept for the combination of acimtamig with allogeneic NK cells in our AFM13-104 study in Hodgkin and non-Hodgkin lymphomas in collaboration with MD Anderson Cancer Center.
We initiated our Phase II LuminICE-203 trial of innate cell engager acimtamig in combination with the off-the-shelf NK cell product AlloNK®. We received encouraging feedback from the US Food and Drug Administration (FDA) on the trial design and potential for accelerated approval. We have now already treated the first patients and are expecting the first results from this study in the first half of 2024.
What were two key findings from the investigational study?
AH: The most important findings from the AFM13-104 study of acimtamig plus allogeneic NK in Hodgkin lymphoma, are the unprecedented response rates and that this was achieved in very advanced stage patients who have failed prior chemotherapy and were double-refractory to BV and CPIs.
One third of patients with a complete response remain free of tumour for more than a year and some patients are without recurrence of their lymphoma for two years”
in a patient population that has failed their previous line of therapy, you are not expecting meaningful responses. In fact, no patient in the AFM13-104 study had a response to the treatment that was given prior to enrolment into the study. To see this magnitude of responses in terms of overall response rate (97 percent) and complete response (78 percent), is unprecedented. Furthermore, we have now seen that one third of patients with a CR remain free of tumour for more than a year and some patients are without recurrence of their lymphoma for two years.
These efficacy results, combined with the safety profile that allows patients to complete their treatment regimen, are extremely encouraging.
Can you share some highlights from the data presented at ASH 2023?
These are unprecedented results in a patient population that had exhausted current standard of care options”
AH: In 32 HL patients treated at the recommended phase 2 dose level (RP2D), the ORR was 97 percent, and the CR rate was 78 percent, with many responses still ongoing. In this cohort median EFS was 9.8 months with 84 percent of patients alive at 12 months, and a median DOR of 8.8 months. Additionally, 30 percent of patients have a long-term response of more than 12 months.
These are unprecedented results in a patient population that had exhausted current standard of care options, having been heavily pretreated with a median of seven prior lines of treatments and all double refractory to BV and CPIs.
Importantly, the treatment was well tolerated with no instances of cytokine release syndrome, graft versus host disease, and neurotoxicity.
What were two of the key challenges in developing the innate cell engagers?
Our first challenge was finding the right partner to provide a scalable, off-the-shelf NK cell product”
AH: After establishing proof of concept for acimtamig+NK cells, our first challenge was finding the right partner to provide a scalable, off-the-shelf NK cell product. Following an extensive evaluation of potential partners, we chose Artiva, Inc. to combine our clinical programmes (Affimed’s acimtamig and Artiva’s AlloNK®) to address the high unmet need for CD30-positive lymphoma patients. AlloNK® is a cryopreserved, off-the-shelf, non-genetically modified, allogeneic cord blood-derived NK cell manufactured at large scale. In preclinical studies, the combination of acimtamig and AlloNK® demonstrated potent anti-tumour activity.
The second challenge was to bring this new combination into the clinic. The IND for the combination was cleared in May 2023 and we have now treated patients in the first two cohorts. In addition, we have received Fast Track designation by the FDA in September 2023 highlighting the impact this combination treatment can have for patients.
What three main factors do you foresee impacting biologics, or more specifically antibody development in the next five years?
We also believe that bispecifics will further establish themselves as an important drug class in the treatment regimens for both haematological malignancies and solid tumours.
Another important factor that will guide the development of new biologics and their success will be their safety profiles and how well they perform in combination in heavily pre-treated, refractory patient populations.
While we’ve been discussing blood cancer today, our approach also has promise in solid tumour settings. In fact, in parallel to our AFM13-104 data update, we announced data from a Phase I/II study of our innate cell engager, AFM24, in combination with the PD-L1 atezolizumab in 15 heavily pre-treated EGFR-Wt non-small cell lung cancer (NSCLC) patients. All patients have been resistant to a CPI.
Results show that in the right setting and with the right combination…innate cell engagers, can provide meaningful benefits for patients”
Responses were observed in four patients, including two confirmed PRs, one unconfirmed CR and one unconfirmed PR awaiting confirmation; an additional seven patients exhibiting stable disease (SD) leading to a disease control rate of 73 percent. Tumour shrinkage was observed in seven (47 percent) patients. The majority of patients experienced only mild to moderate treatment-related adverse events, confirming a well-manageable safety profile.
These results show that in the right setting and with the right combination, biologics, specifically innate cell engagers, can provide meaningful benefits for patients. We firmly believe that this will be solidified in the coming years.
About the interviewee
Dr Andreas Harstrick joined Affimed as CMO in 2020, bringing with him more than 30 years of experience and expertise in cancer drug development, clinical trial research, and regulatory approvals. Prior he was the CMO and member of the management board at Molecular Partners, where he successfully transitioned several preclinical programmes to first-in-human studies. Andreas held several senior executive roles, including Senior Vice President of Medical Sciences at ImClone Systems, Inc., later acquired by Eli Lilly and Company. Before joining ImClone, he was the Senior Vice President of the Global Clinical Development Unit, Oncology, at Merck Serono. Dr Harstrick received his M.D. at the Hannover Medical School, Germany, and spent his career as a practicing oncologist. Additionally, he was an Associate Professor for Internal Medicine at the University of Essen, Germany.
Related topics
Anti-Cancer Therapeutics, Antibodies, Biopharmaceuticals, Drug Development, Drug Safety, Immunotherapy, Research & Development (R&D)
Related organisations
Related diseases & conditions
Hodgkin lymphoma, non-small cell lung cancer (NSCLC), Peripheral T-cell lymphoma









