Trial to assess anti-CD14 antibody as treatment for hospitalised COVID-19 patients
Posted: 14 April 2021 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
The trial will evaluate whether the novel IC14 anti-CD14 antibody can reduce recovery time and severity of COVID-19 symptoms in hospitalised patients.
The US National Institute of Allergy and Infectious Diseases (NIAID) has begun testing the safety and efficacy of a novel anti-CD14 antibody, called IC14, in patients hospitalised with respiratory disease and low blood oxygen due to infection with SARS-CoV-2, the virus that causes COVID-19.
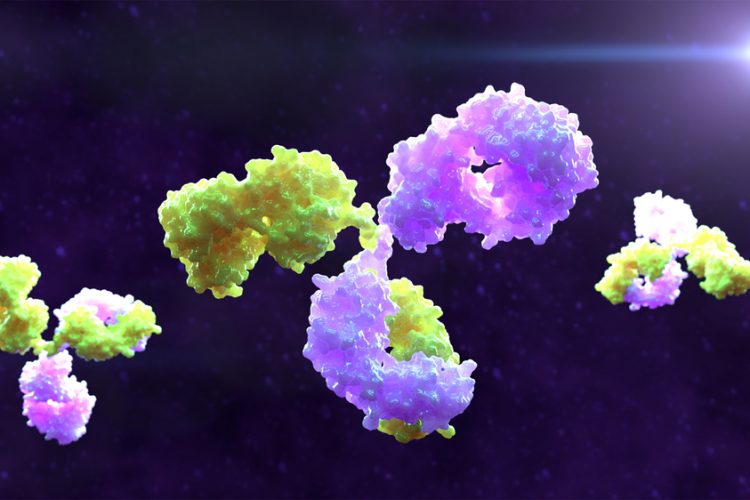
The Phase II COVID-19 anti-CD14 Treatment Trial (CaTT, NCT04391309) will assess whether treatment with the laboratory-created monoclonal antibody can prevent the cytokine storms which are believed to cause the severest symptoms of COVID-19, including Acute Respiratory Distress Syndrome (ARDS), respiratory and multi-organ failure.
IC14 binds to a human protein called CD14 that is found on the surface of immune cells circulating in the blood and airway fluid. CD14 helps immune cells recognise pathogens and injured or dying cells, prompting them to respond. Research suggests that during SARS-CoV-2 infection in the lungs, CD14 overamplifies the later stages of the immune response to the virus, potentially leading to a hyperactive inflammatory response and a cytokine storm. A cytokine storm is a severe immune reaction in which the body rapidly releases numerous immune reaction promoting proteins, called cytokines, into the blood and tissues, resulting in dangerous levels of inflammation and tissue damage.
The CaTT study will enrol 300 to 350 hospitalised COVID-19 patients aged 18 years or older at up to 15 sites nationwide. Volunteer participants will be randomly assigned to receive intravenous infusions of either IC14 or a placebo for four days. As part of the double-blind protocol, all participants will also receive intravenous infusions of the antiviral drug remdesivir for five consecutive days. The study team will follow participants for 60 days with results expected in early 2022.
The main goal of the CaTT study is to determine whether treatment with IC14 decreases the time it takes people with COVID-19 respiratory disease to recover such that they no longer need ongoing medical care in the hospital. Secondary goals are to determine the safety of IC14 in the study population and the efficacy of the drug at reducing the severity of COVID-19. If the results of the CaTT study are promising, then IC14 may be tested in a larger Phase III efficacy trial.
Leading the CaTT study are protocol co-chairs Dr Mark Wurfel, professor of medicine, and Dr Thomas Martin, emeritus professor of medicine, in the Division of Pulmonary, Critical Care and Sleep Medicine at University of Washington, US.
Related topics
Antibodies, Biologics, Clinical Trials, Drug Development, Drug Targets, Therapeutics
Related organisations
University of Washington, US National Institute of Allergy and Infectious Disease (NIAID)
Related drugs
Related people
Related diseases & conditions
Acute Respiratory Distress Syndrome (ARDS), Coronavirus, Covid-19, Cytokine storm