Immunotherapy before surgery benefits melanoma patients
Posted: 2 March 2023 | European Pharmaceutical Review | No comments yet
In a Phase II trial, immunotherapy drug pembrolizumab significantly lowered the risk of recurrence for stage III-IV melanoma patients when given before and after surgery.
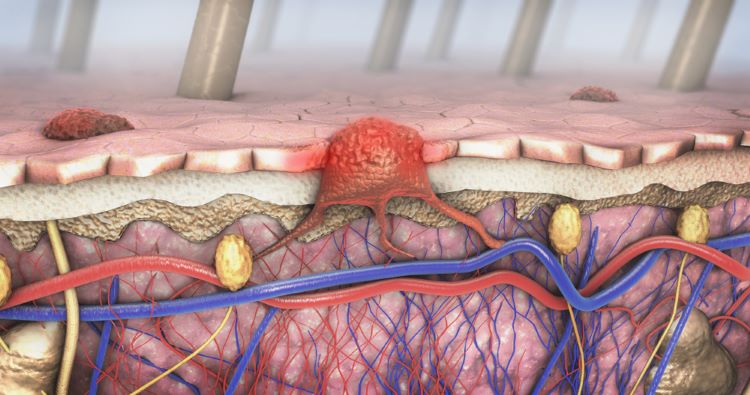
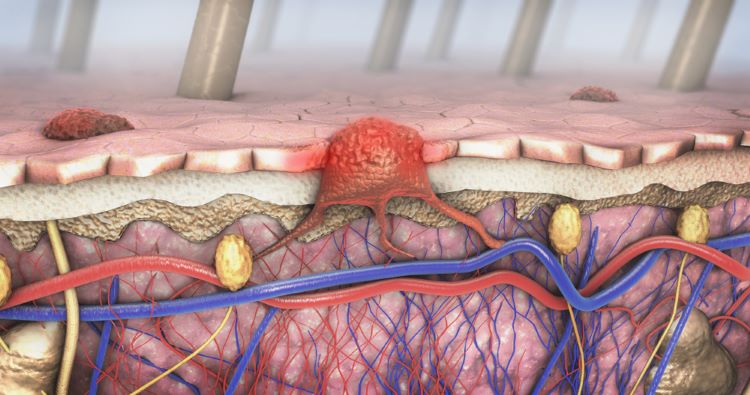
Patients with high-risk melanoma who received immunotherapy drug pembrolizumab both before and after surgery had a significantly lower risk of their cancer recurring than similar patients who received the drug only after surgery, according to a new study.
An immune checkpoint inhibitor, pembrolizumab may help the body’s immune system attack cancer and may interfere with the ability of tumour cells to grow and spread.
The researchers hypothesised that there would be a larger anti-tumour immune response and longer immunologic memory if pembrolizumab was administered while the melanoma tumour was still in the body as opposed to after it had been removed.
Results from the study were published in the New England Journal of Medicine and presented at the European Society for Medical Oncology (ESMO) Congress 2022.
The randomised Phase II study, S1801, enrolled 345 participants with stage IIIB through stage IV melanoma that was deemed operable. Participants aged 18-90 received either surgery followed by 200mg of immunotherapy pembrolizumab every three weeks for a total of 18 doses, or 200mg of pembrolizumab every three weeks for three doses leading up to surgery then an additional 15 doses following surgery.
Neoadjuvant nivolumab improves long-term survival for lung cancer
The primary endpoint measured was the duration of event-free survival. This was defined as the time from randomisation to the occurrence of one of the following: disease progression or toxicity that resulted in not receiving surgery, failure to begin adjuvant therapy within 84 days of surgery, melanoma recurrence after surgery, or death from any cause.
With a median follow-up of 14.7 months, event-free survival was significantly longer in the neoadjuvant-adjuvant therapy arm, with a hazard ratio of 0.58 when compared to the adjuvant therapy arm. This corresponds to a 42 percent lower event rate in the patients receiving the neoadjuvant regimen.
We found that starting treatment before the melanoma is removed – and with it the bulk of tumour-specific T cells – leads to a greater response than giving it after surgery”
“This treatment relies on the presence of pre-existing T cells coming in contact with cancer cells in the body to generate an immune response, and we found that starting treatment before the melanoma is removed – and with it the bulk of tumour-specific T cells – leads to a greater response than giving it after surgery,” noted Sapna Patel, chair of the SWOG Cancer Research Network melanoma committee and Associate Professor of Melanoma Medical Oncology at The University of Texas MD Anderson Cancer Center.
The researchers found that the benefit from neoadjuvant therapy was consistent across a range of factors including patient age, sex, performance status, and stage of disease. Side effects were similar across both arms of the study. Neoadjuvant pembrolizumab did not result in an increase in adverse events related to surgery.
“Future studies can explore de-escalation strategies for both surgery and adjuvant therapy, as well as approaches for patients whose melanoma does not respond to neoadjuvant therapy,” Patel added.
The study (NCT03698019) was led by the SWOG Cancer Research Network, a cancer clinical trials group funded by the National Cancer Institute (NCI). The research was conducted by the NIH-funded National Clinical Trials Network (NCTN). It was sponsored by Merck & Co.
Related topics
Anti-Cancer Therapeutics, Biopharmaceuticals, Clinical Development, Clinical Trials, Drug Safety, Immunotherapy, Research & Development (R&D)
Related organisations
Merck & Co, National Cancer Institute, National Clinical Trials Network, SWOG Cancer Research Network









