Uncovering the cause of immunotherapy resistance in tumours
Posted: 26 July 2017 | European Pharmaceutical Review | 1 comment
Scientists have uncovered a key factor in the development of immunotherapy resistance in the case of cutaneous melanoma. This could potentially lead to future improvements in cancer therapy.
In tumour immunotherapy the body’s own defence system is activated against the tumour cells. However, for the majority of patients, the tumour cells eventually become resistant to the treatments used. Researchers at the University of Zurich and the University Hospital Zurich have now found that in the case of skin cutaneous melanoma an epigenetic control protein is key to the development of this resistance.
Tumour immunotherapy holds promise
Cancer is the second most common cause of death worldwide. Until recently, the chances of cure for patients suffering from metastatic cancer were low, as with such cancer the surgical removal of distant metastases in various organs or their local treatment using radiotherapy were usually unsuccessful. Likewise, the use of chemotherapy is limited by its toxic systemic side effects. Tumour immunotherapy has been used for several years, with patients with certain metastatic cancers showing good responses to this treatment.
These immunotherapies – also called checkpoint inhibitors – allow the body’s own immune system to better detect and destroy the cancer cells, however, over time cancer cells become resistant to the triggered immune responses. Now, researchers at the University of Zurich and the University Hospital Zurich have discovered a mechanism that plays a central role in the development of this resistance.
Immune cells fail to detect resistant cancer cells
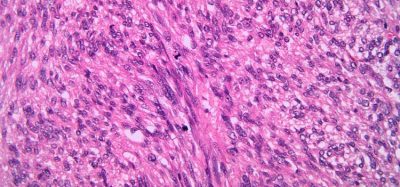
Cancer cells develop resistance by downregulating the features that immune cells use to detect cancer cells. These include tumour antigen presentation by means of so-called MHC class I molecules. These molecules present tumour-specific peptides on the surface of cancer cells so that they become visible to the immune cells, more specifically to T cells. In addition, cancer cells produce specific immune molecules and trigger immunosuppressive processes. The interaction of these changes makes the cancer cells virtually invisible to the immune cells, whereby the immunotherapy becomes ineffective.
“The underlying mechanisms of these changes have been largely unknown until now,” says Lukas Sommer, professor of anatomy at the University of Zurich.”
Ezh2 activity blocking proved successful
The team headed up by Onur Boyman, director of the Department of Immunology at the University Hospital Zurich, has now discovered that the epigenetic control protein Ezh2 plays a central role in how cancer cells develop this resistance. Using animal models, the researchers have demonstrated that the tumour mass initially shrinks during treatment of malignant skin cutaneous melanoma with checkpoint inhibitors or immunostimulating interleukin-2 therapy.
Over time, however, the skin cancer cells produced more Ezh2. As a result, the antigen-presenting MHC class I molecules and the antigens specific to skin cutaneous melanoma were suppressed, while the activity of immunosuppressive modules that curb immune cells simultaneously increased. The skin cancer cells became therefore virtually invisible to the immune system and began reproducing in an uncontrolled manner again.
“As soon as we blocked the activity of the epigenetic regulator Ezh2 with a pharmacological inhibitor, the efficacy of the immunotherapies improved,” says Onur Boyman.
“The tumour masses shrank more significantly and the tumour-free survival was extended.”





Our new small molecules solved this problem.
It is known that tumor cells are weakly immunogenic or non-immunogenic and fail to elicit an efficient protective immune response. It promotes the growth of tumor and justifies the need to enhance the immunogenicity of the cell. Tumor proteins have hydrophilic groups situated on the outer surface of the cell membrane and the hydrophobic – on the inside and hidden with the water content of the cell. Mercureid molecule due to the presence of the atom ion metal in their structure causes deployment of globular protein structures biomembrane (denaturation), which leads to the output of the hydrophobic portions at the outer surface. Conformational changes that result from breaking of intermolecular and intermolecular “hydrogen” bonds when exposed Mercureid lead to change the hydrophobicity of proteins of the outer surface of the cell membrane, increasing the antigenicity and immunogenicity of tumor cells. Proteins undergo denaturation membranes of tumor cells via Mercureid that leads to a redistribution of the outer cell surface peptides in immunogenic clusters and increased expression of MHC molecules on cell surfaces. Denatured proteins become tumor strong stimulators of the immune response as a result of changes in the properties of cell surface antigens.