Unnecessary heart procedures avoided thanks to non-invasive test
Posted: 31 August 2018 | Mike Stones | No comments yet
This is the first study to show the clinical benefit of FFRCT in patients with moderate stenosis, said Dr Bjarne Linde Norgaard of Aarhus University Hospital…
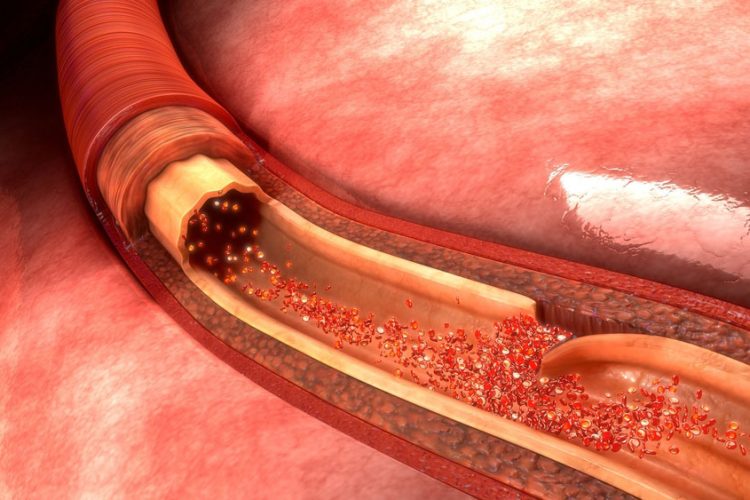
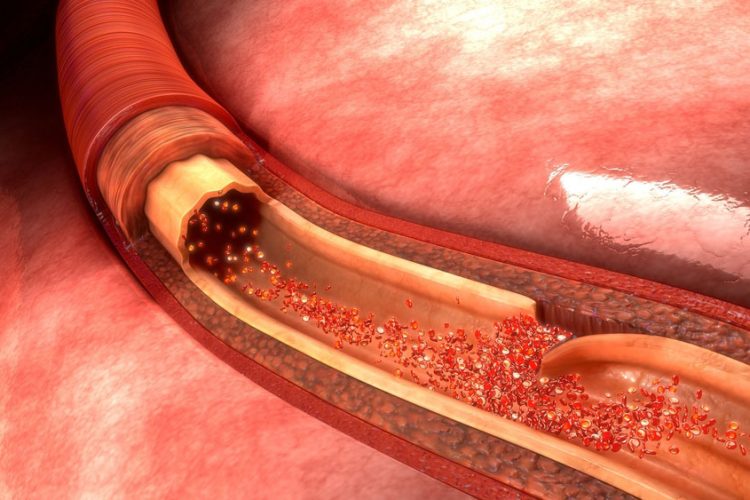
The new non-invasive method identifies which patients with chest pain and clogged coronary arteries, or coronary artery disease, can be treated safely with drugs and do not need invasive diagnostic tests.
Unnecessary heart procedures may be avoided thanks to a non-invasive test studied by researchers at Aarhus University Hospital, Denmark.
Their research, presented at the recent European Society of Cardiology (ESC) Congress, showed that a non-invasive method can be used to identify which patients with chest pain and clogged coronary arteries, or coronary artery disease, can be treated safely with drugs and do not need invasive diagnostic tests.
Chest pain is a warning sign of coronary artery disease, which can cause a heart attack or death if the blockage stops blood flow to the heart. The severity of the blockage and its impact on blood flow determines whether treatment should be drugs, inserting a stent to open the artery, or surgery to replace the artery.
Patients with chest pain are assessed initially with coronary computed tomography angiography (CTA). This is a non-invasive scan that determines the degree of artery narrowing (stenosis), which is expressed as a percentage. The invasive technique known as fractional flow reserve (FFR) is used to assess whether the stenosis is obstructing blood flow – a condition called ischaemia. The FFR procedure involves inserting a pressure wire into the artery to calculate the ratio between the maximum blood flow in the narrowed artery and the maximum blood flow in a normal artery.
Clinical outcomes
The new technique – called FFRCT – uses anatomic information from standard coronary CTA scans and applies a mathematical algorithm simulating blood flow to calculate FFR. The non-invasive method accurately reflects invasively measured FFR, according to several clinical trials. But the researchers reported little information on clinical outcomes using coronary CTA followed by FFRCT to decide treatment.
This is the first study to show the clinical benefit of FFRCT in patients with moderate stenosis, said Dr Bjarne Linde Norgaard of Aarhus University Hospital, Denmark.
“Patients with moderate stenosis on coronary CTA who had normal FFRCT were deemed at low risk of heart attack and received drugs alone,” said Dr Norgaard, who was the principal investigator in the study. “Our study shows that this is a safe strategy, since their prognosis was equally favourable to patients with no or mild stenosis who we know have good outcomes. The findings suggest that coronary CTA followed by FFRCT could be used as a gatekeeper to invasive diagnostic testing, and that patients with moderate stenosis and a normal FFRCT result do not need the invasive test.”
‘Do not need the invasive test’
Patients with abnormal FFRCT (0.80 or less) received medical therapy alone or were referred for invasive coronary angiography, depending on the number of affected arteries and their location. These patients had more severe disease and a less favourable outcome, particularly those who received only medication, said Dr Norgaard. “More research is needed to determine the best management strategy for these patients,” he added.
The study involved 3,674 patients with stable angina who suffered the onset chest pain between 2014 and 2016. All patients had coronary CTA to determine the degree of stenosis. A total of 2,540 patients, less than one third, had mild stenosis and had no additional testing. And 677 patients with moderate stenosis (30–70%) had FFRCT to guide further management. Of those, 410 (61%) patients had normal FFRCT (more than 0.80) and were treated with drugs alone, with no referral to invasive testing or coronary angiography.
Data for the study were supplied by the Western Denmark Cardiac Computed Tomography (WDCT) Registry, the Danish National Patient Registry, and the Civil Registration System.
The research was published in Journal of the American College of Cardiology.
Related topics
Related organisations
Aarhus University Hospital, American College of Cardiology, European Society of Cardiology
Related people
Related diseases & conditions
Clogged coronary arteries, Coronary artery disease, Ischaemia