Merck’s Keytruda®: update on trials and outcomes
Posted: 8 October 2021 | Anna Begley (European Pharmaceutical Review) | No comments yet
EPR’s Anna Begley summarises some of the key results from trials of Merck’s Keytruda® (pembrolizumab) cancer treatment.
Keytruda® reduces risk of cervical cancer death by a third
Merck announced positive results from the pivotal Phase III KEYNOTE-826 trial investigating Keytruda in combination with chemotherapy with or without bevacizumab for the first-line treatment of persistent, recurrent or metastatic cervical cancer.
Keytruda plus chemotherapy (paclitaxel plus cisplatin or paclitaxel plus carboplatin) with or without bevacizumab (Keytruda plus chemo ± bev) reduced the risk of death by 33 percent versus chemotherapy with or without bevacizumab.
Median overall survival (OS) for Keytruda plus chemo ± bev was 24.4 months compared to 16.5 months for chemo ± bev. For the dual primary endpoint of progression free survival (PFS), median PFS was 10.4 months in those treated with Keytruda plus chemo ± bev and 8.2 months among those treated with chemo ± bev. In the trial, Keytruda plus chemo ± bev showed an objective response rate (ORR) of 65.9 percent and chemo ± bev showed an ORR of 50.8 percent.
Median duration of response (DOR) was 18.0 months (range, 1.3+ to 24.2+) in the Keytruda plus chemo ± bev arm and 10.4 months (range, 1.5+ to 22.0+) in the chemo ± bev arm. The results were consistent with or without bevacizumab use.
Disease recurrence or death decreases by 35 percent in Phase III melanoma study
In the Phase III KEYNOTE-716 trial, Keytruda plus chemotherapy reduced the risk of disease recurrence or death by 35 percent compared to placebo. Median relapse-free survival (RFS) had not been reached for either group at the time of this analysis. After 14.4 months follow-up, 11.1 percent of patients on Keytruda had recurrence or died compared with 16.8 percent of patients on placebo, with fewer distant recurrences with Keytruda (4.7 percent) versus placebo (7.8 percent).
KEYNOTE-716 is a randomised, two-part, Phase III trial evaluating Keytruda for the adjuvant treatment of patients with resected high-risk stage II melanoma. The primary endpoint is RFS, and the secondary endpoints include distant metastasis-free survival, overall survival and safety.
In part one of the study, which was double-blind, patients age 12 and older were randomised 1:1 to receive Keytruda, 200mg by intravenous (IV) infusion for adult patients or 2 mg/kg by IV for paediatric patients or placebo every three weeks for up to 17 cycles. In part two of the study, which was open-label, eligible adult and paediatric patients received up to 35 additional cycles of Keytruda. Eligibility for part two included patients who recurred after receiving placebo or completed 17 cycles of Keytruda; patients on Keytruda must not have experienced disease recurrence within six months of completing treatment.
The safety profile of Keytruda was consistent with previously reported studies in patients with solid tumours. Treatment-related adverse events (TRAEs) occurred in 79.9 percent of patients who received Keytruda versus 60.9 percent of patients who received placebo, while Grade 3 or 4 TRAEs were observed in 16.1 percent versus 4.3 percent of patients, respectively.
Keytruda reduces risk of death by 27 percent in breast cancer patients
Keytruda plus chemotherapy reduced the risk of death by 27 percent in patients with metastatic triple-negative breast cancer compared to chemotherapy alone in the Phase III KEYNOTE-355 trial.
There was an increase of 6.9 months in median OS with Keytruda plus chemotherapy compared to chemotherapy alone (23.0 months versus 16.1 months, respectively). Although the trial was not powered to compare efficacy between treatment groups by different chemotherapy regimens, the increase in OS was observed for Keytruda plus chemotherapy across the three chemotherapy choices.
There was no statistically significant difference in OS between the treatment groups in the CPS ≥1 population; due to statistical testing hierarchy, formal testing was not performed in the intention-to-treat (ITT) population.
The incidence of TRAEs was similar among patients in the two treatment groups, with Grade 3-5 TRAEs occurring in 68.1 percent of patients in the Keytruda plus chemotherapy arm and 66.9 percent of patients in the chemotherapy arm. TRAEs led to discontinuation in 18.3 percent of patients in the Keytruda plus chemotherapy arm and 11.0 percent of patients in the chemotherapy arm.
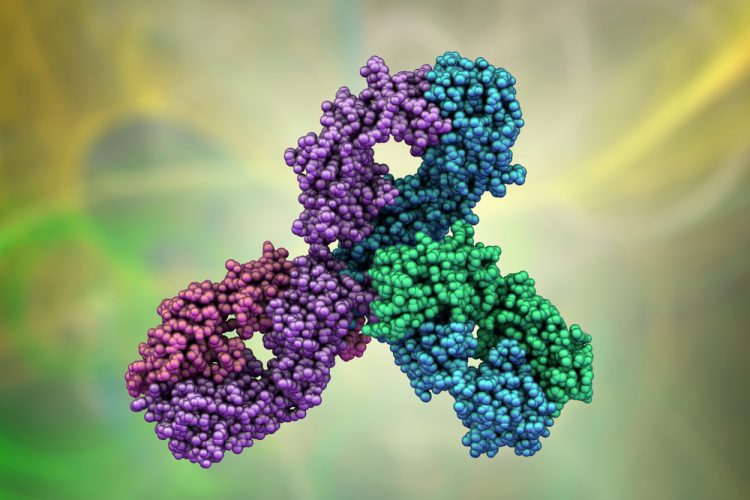
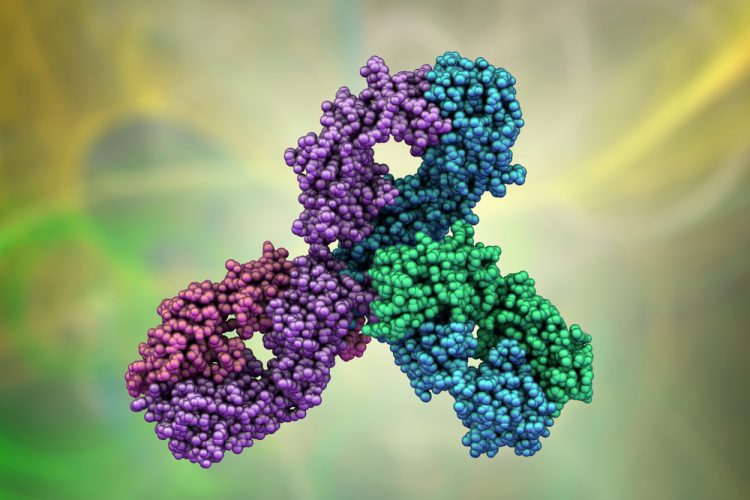
About Keytruda
Keytruda (pembrolizumab) is an anti-programmed death receptor-1 (PD-1) therapy that increases the ability of the body’s immune system to detect and fight tumour cells. The treatment is a humanised monoclonal antibody that blocks the interaction between PD-1 and its ligands, PD-L1 and PD-L2, thereby activating T lymphocytes which may affect both tumour cells and healthy cells.
Related topics
Anti-Cancer Therapeutics, Antibodies, Big Pharma, Biologics, Biopharmaceuticals, Clinical Trials, Data Analysis, Drug Development, Drug Safety, Immunotherapy, Research & Development (R&D), Therapeutics
Related organisations
Related drugs
bevacizumab, carboplatin, cisplatin, Keytruda (pembrolizumab), paclitaxel
Related diseases & conditions
Cervical cancer, Melanoma, metastatic triple-negative breast cancer (mTNBC)









