Application of NGS to enhance the molecular monitoring of CML patients
Posted: 29 April 2024 | ICON Specialty Laboratory Solutions | No comments yet
Q&A with Dr Jin Li and Dr Chad Galderisi of ICON Specialty Laboratory Solutions on how Next Generation Sequencing can support more accurate monitoring of chronic myeloid leukemia patients.
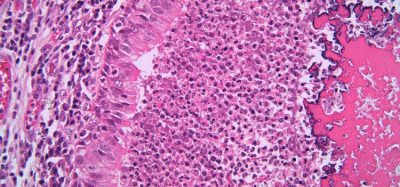
Image credit: ICON
ICON has developed a novel RNA-based Next Generation Sequencing (NGS) assay that supports more accurate monitoring of chronic myeloid leukemia patients. Here we discuss its benefits over standard NGS assays.
What are the main challenges in the molecular monitoring of CML patients?
Approximately 98 percent of chronic myeloid leukemia (CML) patients carry the common e14a2 or e13a2 BCR::ABL1 transcript type, while the remaining have atypical types like e1a2 or e19a2.1 Despite the efficacy of tyrosine kinase inhibitors (TKIs) in treating CML, some patients develop resistance due to mutations in the tyrosine kinase domain (TKD) or myristoyl binding site of BCR::ABL1, depending on the TKI used.2
Managing CML involves identifying the BCR::ABL1 transcript type at diagnosis using multiplex PCR/Sanger or fusion detection NGS assays”
Managing CML involves identifying the BCR::ABL1 transcript type at diagnosis using multiplex PCR/Sanger or fusion detection NGS assays.2 During treatment, monitoring BCR::ABL1 transcript levels via transcript‑specific qPCR (eg, e13/14a2 RT-qPCR on the international scale) and detecting potential TKI resistance mutations via sequencing assays (Sanger or NGS) is crucial.2
The e13/14a2 qPCR assay covers approximately 98 percent of CML patients and is employed for the initial identification of transcript type in some laboratories.2 With over a decade of experience conducting clinical trial testing for CML, ICON Specialty Laboratory Solutions3-5 and other research laboratories2 have observed that relying on qPCR for transcript type determination carries the potential of overlooking atypical transcripts, particularly in cases involving a low level of e13/14a2 combined with elevated expression of atypical transcripts.
ICON and other labs also found that BCR::ABL NGS assays can be sensitive but may yield low-level false positives, posing challenges for high-specificity mutation detection.2,5,6 A recent study suggests a 3 percent variant allele frequency (VAF) cutoff for ABL1 mutation detection to balance specificity and sensitivity, although it may miss mutations below 3 percent VAF, which could be the early sign of TKI resistance.6 VAF levels below 3 percent may be an early sign of TKI resistance and if not detected may result in a missed opportunity for early therapeutic intervention.
What measures can be brought in to help?
An RNA-based NGS assay that addresses the following challenges would significantly benefit the field in the following ways:
- Identification of BCR::ABL1 transcript types (including common and atypical BCR::ABL1 transcripts
- High sensitivity and specificity in mutation detection
- Ability to detect mutations from all transcript types using a single assay
- Simplified molecular testing workflow.
What is ICON doing to help?
ICON Specialty Laboratories developed and validated a novel custom RNA-based NGS assay that enables the identification of BCR::ABL1 transcript type “
To address these challenges, ICON Specialty Laboratories developed and validated a novel custom RNA-based NGS assay (Dup‑Seq BCR::ABL1) that enables both the identification of BCR::ABL1 transcript type (common and atypical) and the detection of resistance mutations from common and atypical BCR::ABL1 transcript types.7
Unlike the standard NGS assay used in the CML field, which requires a minimum 3 percent VAF, this novel assay achieves superior sensitivity and accuracy by detecting mutations with a VAF as low as 1 percent via duplicate PCR and error correction. ICON’s validation study demonstrates that this novel assay achieves high accuracy (PPA for fusion: 98.5 percent; PPA and NPA for mutation at 97.8 percent and 100.0 percent, respectively) and sensitivity (LoD for mutation detection at 3 percent from 10,000 copies of BCR::ABL1 input).
Furthermore, this assay streamlines the molecular testing workflow in the clinical management of CML patients. Its applications in routine clinical workup and clinical trials are diverse. For new CML patients’ routine diagnostic workups, the assay’s transcript typing results can guide the selection of appropriate RT-qPCR for monitoring transcript level changes. However, clinical trial studies usually require baseline transcript type identification and mutation testing, both of which can be addressed by Dup-Seq.
Dup-Seq simplifies the molecular testing workflow in both routine clinical and clinical trial settings
During treatment response monitoring in both settings, Dup-Seq can track the generation and evolution of resistance mutations. While transcript type identification may not be essential for monitoring, it serves as a quality control measure; for instance, a transcript type change during treatment may signal a sample mix-up and prompt repeat testing. In summary, Dup-Seq simplifies the molecular testing workflow in both routine clinical and clinical trial settings, consolidating multiple assays (one transcript type identification assay and a few mutation assays for different transcript types) into a single comprehensive test for efficient management of CML patients.
For further information, visit: ICONplc.com/labs
About the Interviewees

Dr Jin Li is Senior Director, Scientific Affairs, ICON Specialty Laboratory Solutions.


Dr Chad Galderisi is Vice President and Global Medical Director, ICON Specialty Laboratory Solutions
References
- Baccarani M, Castagnetti F, Gugliotta G, et al. The proportion of different BCR-ABL1 transcript types in chronic myeloid leukemia. An international overview. 2019;33:1173-83.
- Cross NCP, Ernst T, Branford S, et al. European LeukemiaNet laboratory recommendations for the diagnosis and management of chronic myeloid leukemia. Leukemia. 2023;37:2150-67.
- Li J, Liu W, Yan Z, al. Next-Generation Sequencing of the BCR-ABL1 Kinase Domain and Neighboring Domains Associated with Therapy Resistance. Blood. 2012; 120 (21): 2549.
- Li J, Yan Z, Darwanto A, al. Phasing Analysis Of TKI Resistance Mutations In The BCR-ABL1 Kinase Domain and Neighboring Domains Using Next-Generation Sequencing. Blood. 2013; 122 (21): 3817.
- Deininger MW, Hodgson JG, Shah NP, et al. Compound mutations in BCR-ABL1 are not major drivers of primary or secondary resistance to ponatinib in CP-CML patients. Blood. 2016;127:703-12.
- Soverini S, Bavaro L, De Benedittis C, et al. Prospective assessment of NGS-detectable mutations in CML patients with nonoptimal response: the NEXT-in-CML study. Blood. 2020;135:534-41.
- Li J, Yan Z, Shi L, et al. Co-detection of BCR::ABL1 common and atypical fusion and mutation using a novel NGS assay, Dup-Seq BCR-ABL1. AACR 2024 abstract 341.