Pioneering AAV gene therapy for Krabbe disease
Posted: 30 May 2024 | Catherine Eckford (European Pharmaceutical Review), Dr Maria Escolar (Forge Biologics) | No comments yet
Dr Maria Escolar, Chief Medical Officer, Forge Biologics, explores the advantages of the company’s novel AAV gene therapy for Krabbe disease, which could help to overcome some of the immune and safety challenges the gene therapy sector is facing.
What makes AAV gene therapies promising when compared to other gene therapies?
A distinguishing factor of AAVs compared to other delivery methods for gene therapies is low incidence of toxicity in humans”
Safety, long-term expression, targeted delivery, versatility, and clinical success of adeno-associated virus (AAV) gene therapies make them a promising approach for treating a wide range of genetic diseases.
A distinguishing factor of AAVs compared to other delivery methods for gene therapies is low incidence of toxicity in humans and less risk for integration with the potential of mutational oncogenesis.
AAV vectors allow for stable and long-term expression of the therapeutic gene. AAVs can target specific tissues or cells making them effective as a delivery mechanism.
Since they are easily modified, this means personalised gene therapies can be developed to suit the needs of individual patients or diseases.
AAV suit a variety of drug delivery methods, including intravenous, intraparenchymal and intrathecal.
What are two of the main immunological safety challenges in traditional AAV gene therapies (without transplantation)?
Although AAVs are generally considered safe well-tolerated compared to other viral vectors, some patients may still develop immune responses against the AAV vector itself, reducing the efficacy of the gene therapy and limiting its long-term benefits, as well as impacting the effectiveness of the gene delivery.
There could also be a cellular immune response to the transgene product. In some cases, the therapeutic protein produced by the transduced cells may be recognised as foreign by the immune system, leading to an immune response against the transgene product.
This immune response can result in inflammation, tissue damage, or the destruction of transduced cells, compromising the efficacy of the gene therapy and causing adverse effects in patients.
What is FBX-101 and what is its mechanism of action?
FBX-101 is a first-in-human gene therapy utilising an AAV to deliver a functioning copy of a faulty or missing gene to patients with Krabbe disease, a rare neurodegenerative disorder”
FBX-101 is a first-in-human gene therapy utilising an AAV to deliver a functioning copy of a faulty or missing gene to patients with Krabbe disease, a rare neurodegenerative disorder.
This treatment is delivered intravenously after haematopoietic stem cell transplantation (HSCT) infusion, preferably unrelated cord blood transplantation.
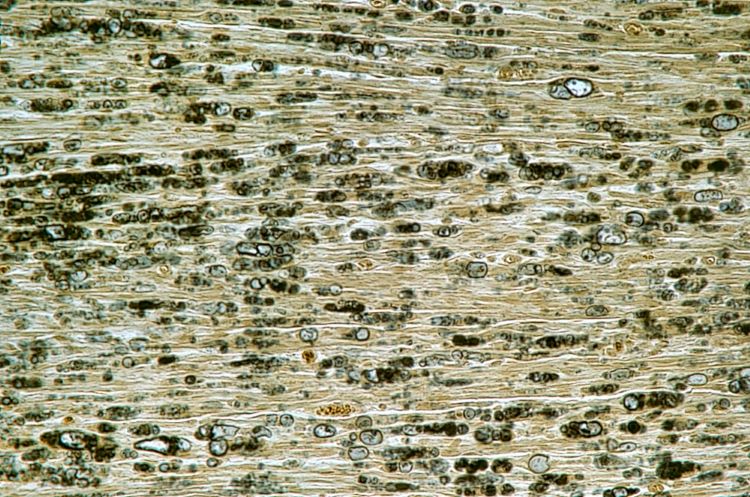
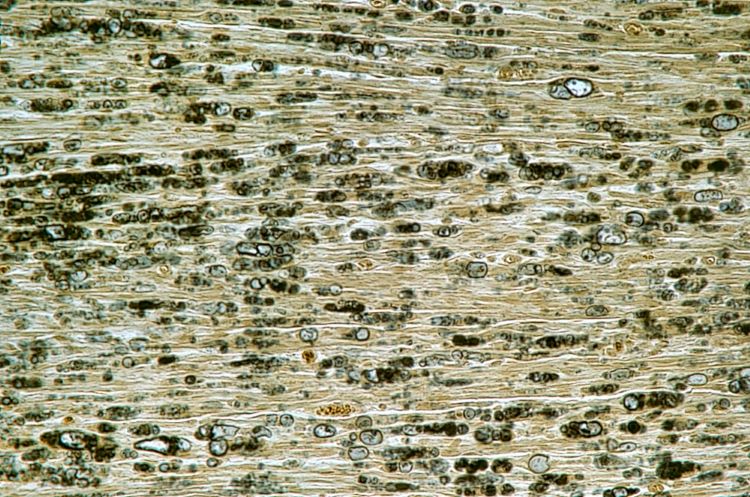
After transplantation, the standard of care, demyelination of the peripheral nervous system continues because there does not seem to be enough enzyme produced by the graft.
With AAV, the vector delivers a functional copy of the galactocerebrosidase (GALC) gene to cells in the peripheral and central nervous system (PNS), and brain (CNS) which increases the expression of GALC enzyme within these cells. The presence of functional GALC enzyme allows for the breakdown of the accumulated toxic substances, such as psychosine, thereby slowing down or halting the progression of the disease.
[FBX-101] treatment in five patients has shown to be safe and well tolerated to date… all patients have been observed walking, a remarkable result”
Treatment in five patients has shown to be safe and well tolerated to date, and to improve myelination and gross motor function. Mobility is the most significant result, and all patients have been observed walking, a remarkable result.
This approach also has the potential to overcome some of the immunological safety challenges observed in traditional AAV gene therapies and extend the duration of gene transfer.
The REKLAIM Phase I/II trial is studying children with asymptomatic infantile and symptomatic late infantile Krabbe disease to investigate the safety and efficacy of a single intravenous infusion of FBX-101 administered more than 21 days after HSCT, the current standard of care.
Why is it a novel treatment for Krabbe disease?
FBX-101 represents a promising and innovative approach to treat Krabbe disease by targeting the underlying genetic cause of the disorder and potentially offering disease-modifying effects.
The current standard of care, HSCT, has been shown to stabilise cognitive decline and significantly improve long-term neurological outcomes. However, HSCT does not correct the peripheral neuropathy that is progressive as the patient grows, leading to loss of gross motor skills and eventually death.
By administering the AAV intravenously during the immune/myeloablation used for transplantation, the patient immune system does not respond to the capsid of the vector.
Therefore, the immune response is either absent or much weaker, improving effectiveness and safety of AAV. This approach can be used as a platform for any other disease in which transplantation is standard of care (other lysosomal storage disorders).
Is there potential for the therapy to be used for other indications? If so, what are some of the key considerations?
FBX-101 has demonstrated significant increases in AAV into the target tissues in the body after HSCT compared to AAV treatment alone”
FBX-101 has demonstrated significant increases in AAV into the target tissues in the body after HSCT compared to AAV treatment alone. This approach helps solve some of the immune challenges faced in gene therapy field.
For use of the gene therapy in other indications, these should be diseases with a well-defined gene or genes responsible for the disease because gene therapy is most effective when it can address a specific genetic defect.
While targeting the CNS with FBX-101 for Krabbe disease is crucial, for other indications, such as muscular dystrophies or metabolic disorders, different tissues may need to be targeted.
How do you think AAV gene therapy development will progress in the future?
The future of AAV gene therapy development is promising and has the potential to revolutionise the treatment of a wide range of diseases by addressing their underlying genetic causes and providing targeted, long-lasting therapeutic benefits.
The progression of AVV technologies is expected to advance as quickly as the biotech industry is advancing and can include enhanced vector design, novel delivery methods, the integration of gene editing capabilities and combination therapies.
Investment in research, continued and increased collaboration between academia and industry and with regulatory agencies, as well as meaningful engagement with patient communities are key.
About the interviewee


Her translational research focuses on prospectively studying the natural progression of rare genetic neurodegenerative diseases and developing treatments.
She has contributed to the design of multiple trials and has been the lead investigator on many gene therapy and enzyme replacement therapy trials.
Dr Escolar is a graduate of the Escuela Colombiana de Medicina. She has a MS in human nutrition from Columbia University and completed a residency in general paediatrics and fellowship in child development and behavioral pediatrics at the Cornell University Medical Center.
Related topics
Biologics, Biopharmaceuticals, Clinical Development, Clinical Trials, Data Analysis, Drug Development, Drug Safety, Gene therapy, Industry Insight, Research & Development (R&D), Technology, Viruses