MS treatment trial to compare stem cell transplantation to biologic drugs
Posted: 13 January 2020 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
The BEAT-MS trial aims to compare the experimental autologous hematopoietic stem cell transplantation (AHSCT) therapy to the best available biologic therapies for multiple sclerosis (MS).
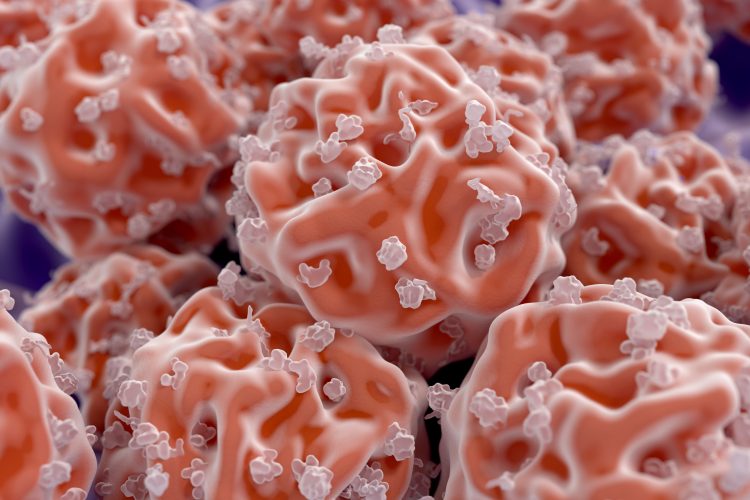
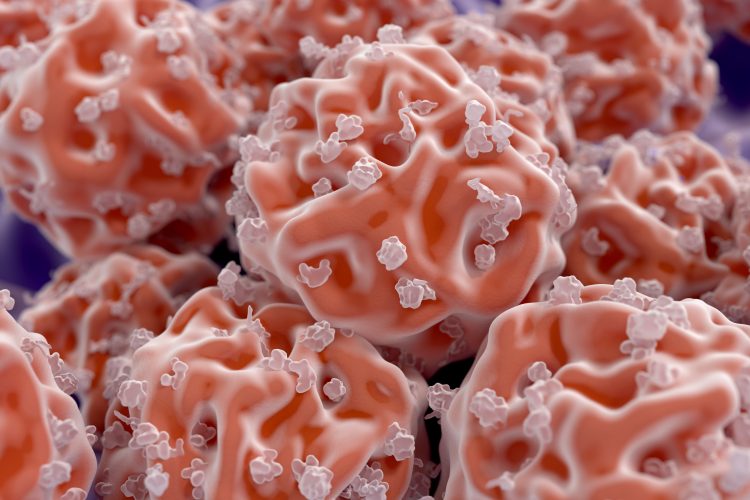
A clinical trial, testing autologous hematopoietic stem cell transplantation (AHSCT) against the best available biologic therapies for severe forms of relapsing multiple sclerosis (MS), has begun. The trial, sponsored by the US National Institute of Allergy and Infectious Diseases (NIAID), aims to assess whether the potential benefits of AHSCT outweigh the risks, ascertaining if it is a viable therapeutic option.
AHSCT has been proposed by previous studies as a possible treatment for MS. The experimental treatment involves using a mixture of four chemical agents to remove autoimmune cells and then reinfusing some of the patient’s own blood-forming stem cells, extracted before treatment, to repopulate the immune system. Immune repopulation theoretically allows the system to reset itself and no longer attack the central nervous system. However, AHSCT has severe side effects, including death.
“AHSCT has the potential to halt the progress of relapsing MS, eliminate the need for a person to take lifelong medication and allow the body to partially regain function. However, we need to be certain that the benefits of this form of treatment outweigh its serious risks,” said NIAID Director Dr Anthony Fauci.
The trial, called BEst Available Therapy versus autologous hematopoietic stem cell transplant for Multiple Sclerosis (BEAT-MS), is being conducted by the Immune Tolerance Network (ITN) in collaboration with the Blood and Marrow Transplant Clinical Trials Network (BMT CTN), both funded by components of the National Institutes of Health (NIH).
BEAT-MS will enrol 156 adults aged 18 to 55 years across the US and UK. In the double-blind trial, participants will be randomly assigned to receive either AHSCT or one of the best available high-efficacy biologic drugs. Neurologists will then periodically examine the participants and assess their level of disability over the following six years.
The investigators will:
- measure how much time elapses between a participant’s assignment to a treatment strategy and MS relapse or death from any cause
- investigate the mechanisms of action of the two treatment strategies and compare the developing immune systems of AHSCT recipients with the immunologic features of participants who receive the biologic drugs
- compare the effects of the treatments on other measures of disease activity and severity; cost-effectiveness in terms of health care costs and individual productivity; and participants’ quality of life.
“We hope that BEAT-MS will clarify the best way to treat people with relapsing MS,” concluded trial leader Dr Jeffrey Cohen, director of the Experimental Therapeutics Program in the Mellen Center for Multiple Sclerosis Treatment and Research at the Cleveland Clinic.
Related topics
Clinical Trials, Drug Development, Research & Development (R&D), Stem Cells
Related organisations
Blood and Marrow Transplant Clinical Trials Network (BMT CTN), Immune Tolerance Network (ITN), Mellen Center for Multiple Sclerosis Treatment and Research at the Cleveland Clinic, US National Institute of Allergy and Infectious Diseases (NIAID), US National Institutes of Health (NIH)