Using albumin could facilitate vaccination by inhalation, finds pre-clinical study
Posted: 23 March 2021 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
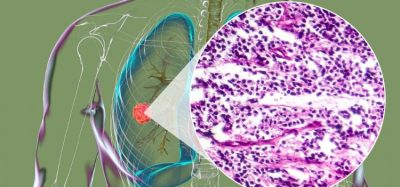
MIT researchers developed and tested in mice intratracheal vaccines to protect against the vaccinia virus and the formation of lung cancer.


Researchers have developed a new vaccination strategy to protect against viruses, such as SARS-CoV-2 (which causes COVID-19), that infect hosts via mucosal surfaces like the lining of the respiratory tract.
In their pre-clinical study, the Massachusetts Institute of Technology (MIT) researchers demonstrated that their inhaled vaccination method can induce a strong memory T-cell response in the lungs of mice. Their strategy delivers a peptide vaccine modified to bind to albumin, a host protein naturally present in mucus, which can ferry the vaccine across the mucosal barrier to induce an immune response.
“In this paper, we specifically focused on T-cell responses that would be useful against viruses or cancer and our idea was to use this protein, albumin, as sort of a Trojan horse to get the vaccine across the mucosal barrier,” explained Darrell Irvine, the senior author of the study, who is the Underwood-Prescott Professor with appointments in the departments of Biological Engineering and Materials Science and Engineering; an associate director of MIT’s Koch Institute for Integrative Cancer Research; and a member of the Ragon Institute of Massachusetts General Hospital (MGH), MIT and Harvard University, all US.
In addition to protecting against pathogens that infect the lungs, the researchers stated that these inhaled vaccines could also be used to treat cancer metastasising to the lungs, or even prevent tumours developing in the first place.
Overcoming the mucosal barrier
The team decided to pursue the use of peptide vaccines, which are thought to be safer and known to be easier to manufacture than the live, attenuated viral vaccines which are currently approved for nasal or oral administration. However, they are also more difficult to get across mucosal barriers.
To overcome this, the team turned to an approach which they had studied in a 2014 paper. In that research, Irvine et al. observed that attaching peptide vaccines to serum albumin proteins helped the peptides to accumulate in the lymph nodes, where they could activate a strong T-cell response.
Those vaccines were given by injection; however, in their new study, the team investigated whether albumin could also help peptide vaccines get across mucosal barriers such as those surrounding the lungs. They chose albumin because of its role in helping to maintain osmotic pressure in the lungs and its ability to easily pass through the epithelial tissue surrounding the lungs.
To test their theory, the researchers attached an albumin-binding lipid tail to a peptide vaccine against the vaccinia virus. The vaccine also included a commonly used adjuvant called CpG.
The vaccine was delivered intratracheally, which simulates inhalation exposure. The investigators reported that this method of delivery generated a 25-fold increase in memory T cells in the mouse lungs, compared to an intramuscular injection of the albumin-modified vaccine. They also showed that when mice were exposed to the vaccinia virus months later, the intramuscular vaccine offered no protection, while all the animals that received the vaccine intratracheally were protected.
Vaccinating against lung tumours
The researchers also tested a mucosal vaccine against cancer. They vaccinated mice using a peptide found on melanoma. When the vaccinated mice were exposed to metastatic melanoma cells, T cells in the lungs were able to eliminate them. Additionally, the team demonstrated that the vaccine could help to shrink existing lung tumours.
According to Irvine, this kind of local mucosal response could make it possible to develop vaccines that would prevent tumours from forming in specific organs, by targeting antigens commonly found on tumour cells.
He concluded that the same strategy could also be useful for creating mucosal vaccines against other viruses such as HIV, influenza or SAR-CoV-2 and that his lab is now using it to develop a vaccine able to induce a potent antibody response against SARS-CoV-2.
The study was published in Science Immunology.
Related topics
Anti-Cancer Therapeutics, Biologics, Drug Delivery Systems, Drug Development, Immunisation, Research & Development (R&D), t-cells, Vaccine Technology, Vaccines, Viruses