Checkpoint inhibitor combination shows promise in Merkel cell carcinoma
Posted: 13 September 2022 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
Dual checkpoint inhibitor blockade could be a promising first-line and salvage therapeutic option for advanced Merkel cell carcinoma, say researchers.
Researchers suggest an investigational combination therapy could offer a new therapeutic option for Merkel cell carcinoma patients who may not respond to the current standard of care.
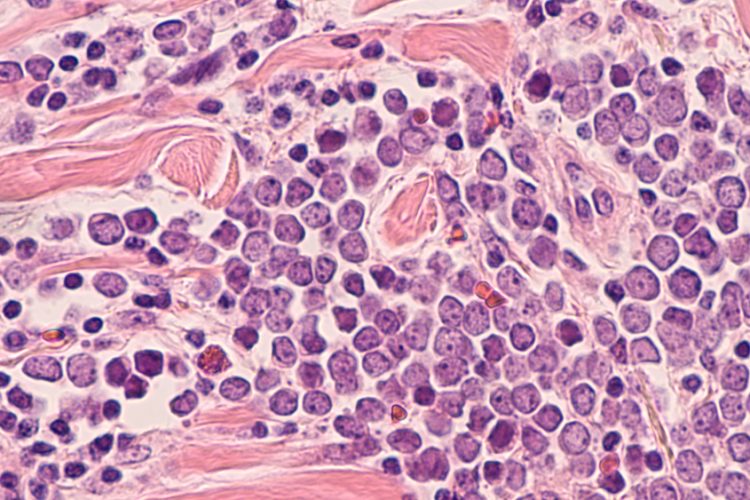
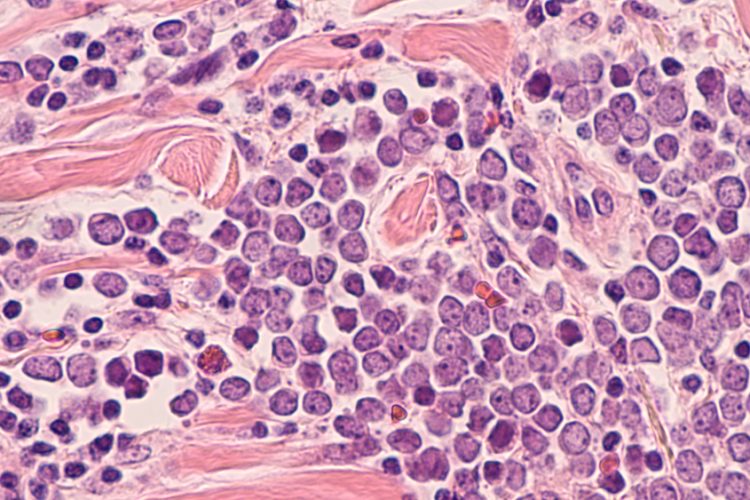
Merkel cell carcinoma is a rare but aggressive form of skin cancer that has a high rate of metastasis and poor patient outcomes. The current standard of care for patients with recurrent, unresectable or metastatic disease is immune checkpoint inhibitor monotherapy targeting anti-programmed death receptor 1 (anti-PD-1) and programmed death ligand 1 (PD-L1), but only about half of patients respond to this therapy.
In the trial (NCT03071406), 50 patients with unresectable, recurrent or stage 4 Merkel cell carcinoma were randomly assigned to two treatment groups:
- received a combination of ivolumab 240mg intravenously every two weeks plus ipilimumab 1 mg/kg intravenously every six weeks; and
- received the ipilimumab and nivolumab combination along with stereotactic body radiation therapy (24 Gy in three fractions at week 2).
Ipilimumab is a checkpoint inhibitor targeting cytotoxic T lymphocyte-associated antigen 4 (CTLA4) and nivolumab is an anti-PD-1/ PD-L1 inhibitor.
Both groups included a mix of patients who had and had not previously been treated with immune checkpoint inhibitor therapy targeting anti-PD-1/ PD-L1. The primary endpoint for this phase of the trial was objective response rate (ORR), defined as the percentage of patients whose tumours decreased or disappeared after receiving the therapy.
Results presented at the European Society for Medical Oncology Congress (ESMO) reveal that, regardless of the treatment group, all 22 patients who had not received previous immune checkpoint inhibitor therapy responded to the investigational combination therapy, with 41 percent having a complete response. Moreover, in the 26 patients who had previously been treated with immune checkpoint inhibitors, eight responded to therapy with four having a complete response.
The addition of stereotactic body radiation therapy did not improve efficacy of the nivolumab and ipilimumab combination therapy.
Based on the data, the researchers stated that “the combination of nivolumab and ipilimumab represents a new first-line and salvage therapeutic option for advanced Merkel cell carcinoma.”
Grade 3 or 4 treatment-related adverse events were observed in 10 (40 percent) of 25 patients in the combination group and eight (32 percent) of 25 patients in the combination plus stereotactic body radiation therapy cohort.
Commenting on the study, Sungjune Kim, MD, PhD, principal investigator of the trial and associate member of the Radiation Oncology Department at the Moffitt Cancer Center, US, stated: “Our results show that first-line combination therapy with nivolumab and ipilimumab has a high overall response rate with durable responses for patients with advanced Merkel cell carcinoma. This presents a new option for patients who may not respond to the current standard of care therapy for this disease.”
The trial was supported by the Bristol Myers Squibb Rare Population Malignancy Program, the National Cancer Institute (K08 CA194273, R37CA248298, P30-CA076292) and the Moffitt Foundation.
The results were also published in The Lancet.
Related topics
Anti-Cancer Therapeutics, Antibodies, Biologics, Clinical Development, Clinical Trials, Drug Development, Research & Development (R&D), Therapeutics









