Study reveals huge improvement for severe HHT patients after bevacizumab treatment
Posted: 31 January 2018 | European Pharmaceutical Review | No comments yet
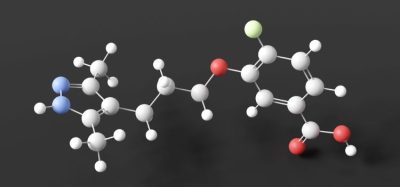
A new study reveals the efficacy and safety of using intravenous bevacizumab to treat patients with severe hereditary haemorrhagic telangiectasia (HHT). Successful results suggest it should be used as a first-line therapy.


HHT – also known as Rendu-Osler-Weber disease – is a rare genetic disorder that affects blood vessels. Individuals with HHT have abnormal blood vessel clusters (referred to as AVMs or telangiectasias) that have a high propensity to rupture and bleed. This can result in haemorrhagic strokes, epistaxis (nose bleeds) and bleeding from the digestive tract. Patients can become severely anaemic and blood transfusion dependent as a result.
Commenting on the symptoms experienced in HHT cases, Vivek N. Iyer, MD, MPH, of the Department of Pulmonary and Critical Care Medicine, Mayo Clinic (Rochester, MN) said: “Some HHT patients suffer from severe epistaxis and gastrointestinal (GI) bleeding, which can result in severe anaemia and years of blood transfusions. Both problems also appear to sometimes worsen with age.
In some patients, both epistaxis and GI bleeding can become refractory/resistant to existing treatment options, leaving patients severely anaemic and dependent on iron infusions or blood transfusions. Quality of life is very poor in these cases.”
HHT study details
Investigators analysed the records of 34 patients who were treated with intravenous bevacizumab for severe HHT-related bleeding at the Mayo Clinic HHT Center of Excellence in Rochester, Minnesota. The records covered a period of 44 months between June 2013 and January 2017. The primary source of bleeding was epistaxis in 15 patients, GI bleeding in four patients, and combined epistaxis and GI bleeding in 15 patients. Most patients had tried to control the bleeding using standard medical and interventional approaches – including ENT laser cauterisation procedures, septodermoplasty and GI endoscopies – but without success.
Red blood cell (RBC) transfusions had been administered to 28 patients. Of these, 16 patients were RBC transfusion dependent and had received a median of 75 RBC transfusions before starting treatment with bevacizumab. The typical initial dosing cycle consisted of eight doses (four doses each administered two weeks apart followed by four doses each administered one month apart) over a period of around 22 weeks.
An Epistaxis Severity Score (ESS) questionnaire was used to assess the severity of nose bleeds at both at the beginning of the study and after starting bevacizumab treatment. Further ‘top up’ or maintenance doses following completion of the initial dosing cycle were individualised in each patient. Patients were instructed to maintain close follow-up with monthly laboratory checks with the aim to re-dose bevacizumab before the bleeding situation had deteriorated significantly.
Resulting ESS scores reduced
One month after starting treatment, ESS scores were significantly reduced and improvement was maintained after completion of the initial bevacizumab treatment cycle. Further ESS score improvements occurred on follow-up, with several patients essentially reporting a complete cessation of nose bleeding after bevacizumab treatment. This is notable, given the severity of symptoms in this group that had already failed to respond to various medical and interventional therapies prior to this treatment. Of the 16 patients who were receiving RBC transfusions before the treatment, only two were still receiving these after the treatment ceased. GI bleeding also similarly improved with resolution or improvement in anaemia in all 19 patients with this condition. Patients experienced few side effects and were followed for an average of about 21 months after starting bevacizumab.
Bevacizumab suggested as first-line option
“Currently, there are no FDA-approved pharmacological treatments available for HHT patients with severe bleeding. This study provides good quality evidence for the excellent efficacy and safety of intravenous bevacizumab in the treatment of these patients.
Intravenous bevacizumab should be considered as a standard, first-line treatment option for HHT patients with severe bleeding and transfusion dependent anaemia,” concluded Dr. Iyer.
James R. Gossage, MD, of Augusta University (Augusta, GA), commented, “Although one can attribute changes in ESS score or quality of life to the placebo effect, it is much harder to attribute so dramatic a change in transfusion requirement to placebo. It is still desirable to have a randomised placebo-controlled trial. However, until we have those data in hand, I agree with Iyer et al that systemic bevacizumab should be considered as a first-line therapy for the treatment of refractory bleeding in patients with HHT.”
The study was published in Mayo Clinic Proceedings.