Psoriasis treatment linked to improvement in heart disease
Posted: 5 February 2019 | European Pharmaceutical Review | No comments yet
Treatments for psoriasis could help prevent heart disease in patients with the skin condition, with patients having an 8 percent reduction in their risk…


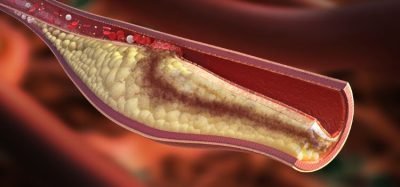
Anti-inflammatory biologic drugs used to treat severe psoriasis have the potential to prevent heart disease in patients with the skin condition. During one year of treatment, biologic therapy improved coronary artery plaque similar to the effect of a low-dose statin.
“Psoriasis severity is related to the burden of coronary disease – our findings suggest treating the psoriasis may potentially benefit coronary heart disease,” said study author Dr Nehal Mehta, Chief of Inflammation and Cardiometabolic Diseases at the National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health (NIH), Bethesda, Maryland, US.
Psoriasis causes scaly skin patches, often on the elbows, knees, scalp, and lower back. Patients with the skin condition have an elevated risk of heart disease – young patients with severe psoriasis are at twice the risk of having a first heart attack at 40-50 years of age.
Psoriasis patients often have inflammation throughout the body and may be treated with anti-inflammatory biologic therapy when their skin condition is severe and topical treatments or phototherapy have failed. This study investigated whether treating severe psoriasis with a biologic could improve the health of the coronary arteries.
The study found that patients with severe psoriasis who took biologic therapy for one year had an 8 percent reduction in total and non-calcified coronary plaque burden, a frequent cause of heart attacks (see figure) – similar to the effect of a low dose statin. The make-up of coronary plaques also improved in those taking biologics, making them less risky. Coronary plaque burden increased by 2 percent in patients who did not take a biologic.
Dr Mehta said: “We found that these anti-inflammatory drugs commonly used to treat severe psoriasis also improve plaque in the coronary artery making them more stable and less likely to cause a heart attack. This occurred in the absence of changes in traditional cardiovascular risk factors including blood pressure and blood lipids.”
During the one-year study, systemic inflammation assessed by blood markers reduced only in the group taking biologic therapy. Dr Mehta said it is too early to say whether biologics exert their effects on coronary plaques directly or by reducing systemic inflammation.
He said: “This preliminary study provides the first evidence that biologic therapy is associated with coronary plaque reduction and stabilisation,and provides strong rationale for conduct of a randomised trial testing the impact of biologic therapy on the progression of coronary disease in patients with psoriasis.”
Dr Mehta noted that some patients with severe psoriasis opt not to take a biologic medicine because they suppress the immune system and may increase the chance of infection. In addition, they must be injected.
Previous research has shown that in heart attack patients, anti-inflammatory biologic therapy reduces the risk of another cardiovascular event.
“With the results of that study and our current one, my message to patients with psoriasis is to take untreated inflammation seriously,” said Dr Mehta. “When someone has severe psoriasis, they are at higher risk of heart attack and treating the psoriasis may reduce that risk.”
The observational study included 121 patients with severe psoriasis who qualified for biologic treatment. Of those, 89 took biological therapy (one of three types) and 32 used topical treatment. All patients underwent imaging of their coronary arteries with computed tomography angiography at baseline and one year later to assess the amount and characteristics of plaques such as the necrotic core which causes plaque rupture.
The research was published in the journal Cardiovascular Research.
Related topics
Analytical techniques, Clinical Development, Clinical Trials, Drug Development, Research & Development (R&D)