New glioblastoma cancer vaccine shows promise in phase 1b clinical trial
Posted: 1 April 2019 | European Pharmaceutical Review | No comments yet
A brain-cancer vaccine more than 20 years in the making suspends cancer growth in patients enrolled in early-stage trial…
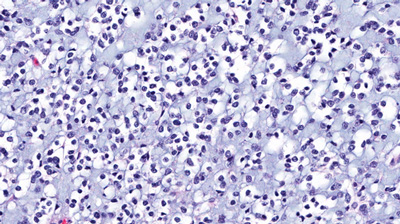
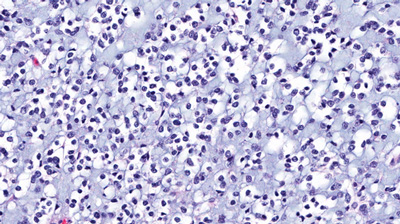
Glioblastoma is the most aggressive type of primary brain cancer, one with a prognosis of 11–15 months with standard treatment. Results from a phase 1b clinical trial of a new experimental glioblastoma vaccine developed by Jefferson and Imvax, show the treatment was tolerated well by patients, slowed tumour recurrence, and prolonged patient survival.
The research was presented at an oral session of the American Association for Cancer Research (AACR) annual meeting on 31 March 2019 in Atlanta, Georgia.
Researchers treated 33 patients with newly diagnosed glioblastoma multiforme with the novel cancer vaccine (IGV-001) in a prospective phase 1b clinical study and compared outcomes to a historical comparator group of 35 patients treated with standard of care at the same institution. The results showed patients treated with the vaccine had improved progression-free survival and overall survival compared to the control group treated with standard of care alone.
“The response we see in some patients is very encouraging,” says Dr David Andrews, Professor of Neurosurgery at the Vickie & Jack Farber Institute for Neuroscience – Jefferson Health and co-founder, Chief Medical Officer and interim Chief Executive Officer of Imvax. “We look forward to initiating a phase II trial later this year to confirm these phase 1b results.”
The vaccine is created from the patient’s own tumour cells sampled during surgical removal of the primary brain tumour. Researchers first take the cancer cells, treat them with an antisense oligodeoxynucleotide (AS-ODN) against IGF-R1, a receptor shown to drive tumour growth and metastasis, and load them with additional AS-ODN into diffusion chambers. Then the dime-sized chambers and their contents are irradiated and implanted under the skin of the patient’s abdomen.
“As a consequence of the combined effects of the IGF-1R antisense and irradiation, our evidence shows that the chambered tumour cells release antigens, which together with the immunomodulatory AS-ODN, diffuse out of the chamber into the patient’s body and activate the immune system against brain tumour cells,” says immunologist Dr Craig Hooper, Professor of Cancer Biology at the Sidney Kimmel Cancer Center – Jefferson Health and a co-founder and Chief Scientific Officer of Imvax.
Dr Andrews was frustrated with the poor options for treatment in glioblastoma. He was interested in using antisense molecules, ones that render glioblastoma cells more susceptible to conventional radiotherapy. However, preclinical experiments and an early clinical study of the effect of implantation of diffusion chambers containing glioblastoma cells showed there was radiographic evidence of delayed tumour shrinkage. This delay suggested that a systemic, possibly immune response may be at play. To better understand the observations, Dr Andrews worked with Dr Hooper, who has an extensive background in studying immune regulation and particular expertise in neuroimmunity.
Over the course of 15 years, translational research led by Dr Hooper and clinical studies led by Dr Andrews refined the diffusion chamber combination product used in the current phase 1b trial.
The phase 1b clinical trial builds on earlier work showing that standard-of-care treatment for glioblastoma damages the immune system and suggesting that the vaccine would be more effective in patients whose immune systems had not been compromised by prior therapy. The phase 1b trial only enrolled patients who were scheduled to have surgery, prior to the start of standard-of-care adjuvant therapy.
The results showed that patients who received the Imvax glioblastoma vaccine had longer progression-free survival and overall survival – two common measures of cancer treatment success – than the control group. The researchers saw no vaccine-related adverse events.
Related topics
Related organisations
Imvax, Sidney Kimmel Cancer Center – Jefferson Health, Vickie & Jack Farber Institute for Neuroscience – Jefferson Health









