Linking health and lifetime exposures through biomarkers in breath
Posted: 28 September 2020 | Dr Jonathan Lawson (Owlstone Medical) | No comments yet
Dr Jonathan Lawson explains why detecting and monitoring exposures and the body’s response from breath could be the key to predicting future health issues.


In recent years, the role of our environment and the factors we encounter throughout our lives has become an increasingly prominent feature in medical research and healthcare, with a number of common exposures, such as particulate matter, now classified as carcinogens by the International Agency for Research on Cancer (IARC). Twenty years ago, the completion of the human genome project held promise for curing every disease, yet what it has served to highlight is the complex, ever-changing environment in which our genes and epigenetic factors operate. While there are few well-established connections between exposure and health – lung cancer and smoking1 or mesothelioma and asbestos,2 for example – many more are yet to be elucidated (Figure 1).
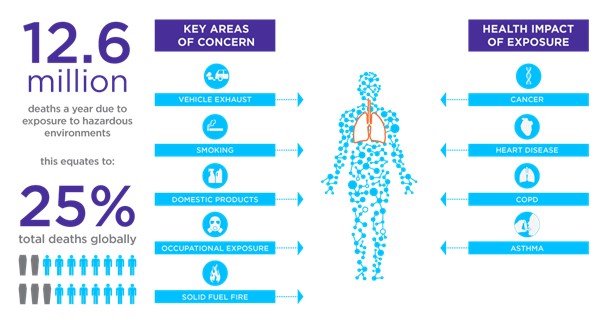
Figure 1: A number of exposure sources are already recognised as having impacts on human health and the contribution of exposures to human deaths is significant.
With increasing pressure on global healthcare systems – an issue thrust into the spotlight in recent months – understanding the impact of environmental exposures on health could hold a vital key to the future of medicine. Uncovering these relationships can help determine those most at risk, reveal the early warning signs of disease development and prevent disease spread by minimising dangerous environmental exposures.
However, achieving this goal is no small undertaking. The effects of exposure can be subtle and it can be years or even decades before symptoms arise, so discovering these connections requires long-running trials based on regular monitoring of test subjects. Moreover, everyone is exposed to a plethora of factors throughout their lives so identifying which ones have health impacts requires a broad range of approaches. This concept has resulted in the emerging field of exposomics.
Exposomics
Why breath?
Breath testing represents one such solution for exposomics. These tests have been applied effectively in selected contexts since the early days of exposure research5,6 and have been used widely in the measurement of benzene and other chemical solvents. The utility of breath tests as a generally palatable approach for regular, non-medical use with the public has already been effectively demonstrated through the use of roadside ethanol breathalysers by the police. Aside from this, with recent technological advances, breath is becoming increasingly recognised as a powerful tool for biomarker detection in exposure as well as medical contexts.
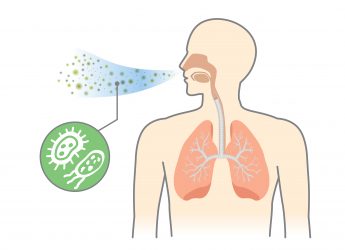
Beyond the obvious atmospheric gases, we now know that exhaled breath contains in excess of a thousand volatile organic compounds (VOCs)7 originating both from inside the body based on an individual’s metabolism and from external sources including diet, medications and environmental exposures (Figure 2). Within the field, VOCs from external sources have often been treated as contaminants to be excluded; however, in the context of exposure they represent a rich source of information about the body’s interaction with the environment and microbiome. Breath also contains respiratory droplets produced as aerosols in exhaled breath. These are created from fluids in the lungs and can contain non-volatile compounds, lipids, proteins, nucleotides and even viruses and bacteria, which can be collected and analysed as an additional source of information.
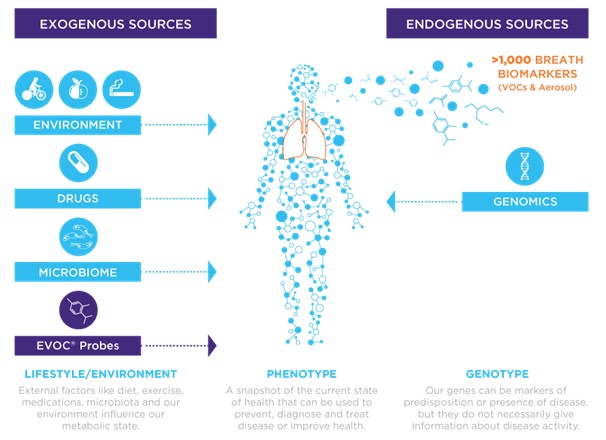
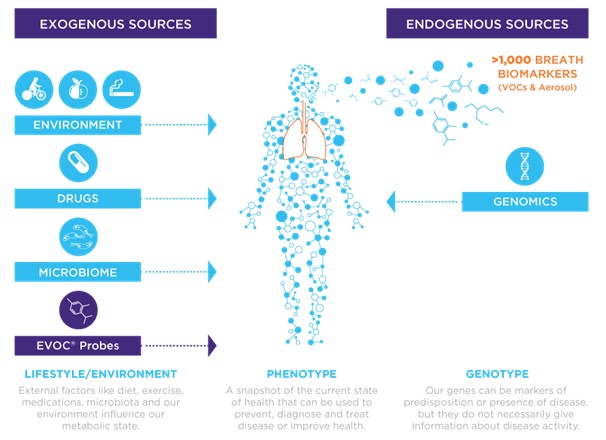
Figure 2: Biomarkers on breath include volatile organic compounds (VOCs) and respiratory droplets. Both can be rich sources of exposure and health information reflecting a combination of endogenous and exogenous factors.
Breath tests therefore can provide a particularly elegant solution for exposure research. One of the great benefits of breath is that it is inexhaustible; you can collect samples from the same person with high frequency, enabling longitudinal studies that simply would not be possible in other fields. Additionally, providing a breath sample is preferred by most patients to giving tissue, blood or stool samples. Furthermore, for exposure research, breath can be used to simultaneously monitor the levels of environmental factors as well as the markers of their effects in the body. This allows for a more direct comparison in an area that has proven particularly challenging.
Emerging technologies
Breath has been a topic of investigation for over 50 years now,8,9 but only recently have the technologies begun to be developed to realise the potential of this rich sampling medium. Standardised sample collection devices that collect breath during regular tidal breathing without the need for training or specialist support are emerging for use across a wide variety of applications. These devices enable the robust collection and storage of high-quality samples suitable for detailed molecular analysis. The reliable identification of VOCs on breath has also progressed rapidly, with high sensitivity mass spectrometers now making it possible to study many VOCs in parallel in concentrations spanning six orders of magnitude.
Breath tests therefore can provide a particularly elegant solution for exposure research”
Modern breath collection approaches typically involve the gathering and pre-concentration of VOCs from exhaled breath onto adsorbent tubes, which contain matrices that trap and hold VOCs. When heated, the tubes release VOCs which are then fed into and analysed using advanced gas chromatography mass spectrometry (GC-MS). The application of advanced data analytics to the resulting spectrograms facilitates the identification of breath biomarkers that can be associated with specific diseases or exposures. There are already technologies available that, combined with the right biomarkers, could enable easy-access, portable breath testing with the ability to provide rapid results in a range of situations.
Given the great power of breath collection for exposure research, it is no surprise that breath research is now becoming integrated into major exposure research consortia. The Exposome Project for Health and Occupational Research (EPHOR) is one of these. Supported by European Horizon 2020 funding, EPHOR unites 19 exposure,10 health and data scientists and technology partners from 12 different countries. This forms just part of the European Human Exposome Network, a conglomerate of nine consortia representing over €100 million of research funds (Figure 3).


Figure 3: A summary of the EPHOR consortium of European organisations aiming to develop a toolbox for the investigation of workplace exposures. The consortium is supported by H2020 funding from the EU. Figure reproduced from.10
Exposure research represents a tangible shift in our approach to health and disease, working to identify factors that contribute to disease as early as possible so they can be mitigated or avoided. Breath testing seems set to play a key role in this approach and it is easy to foresee wide ranging applications across commerce, industry and healthcare where regular breath testing could help us to identify and avoid excessive risks, improving long-term health and ultimately reducing the burden on healthcare systems.
About the author
Dr Jonathan Lawson holds a PhD in Genetics and Developmental Mechanisms from the University of Cambridge and is currently the Head of Content at Owlstone Medical. Most recently he has been working on the third edition of Breath Biopsy: The Complete Guide, an introduction to the field of breath research. He is passionate about sharing the latest science with a wide range of audiences and believes in the benefits of evidence-based research.
References
- What are the Risk Factors for Lung Health? [Internet]. CDC. [cited 17 June 2020]. Available from: https://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm
- McDonald JC, McDonald AD, The epidemiology of mesothelioma in historical context. European Respiratory Journal. 1996; 9: 1932–1942.
- Wild CP, Complementing the Genome with an “Exposome”: The Outstanding Challenge of Environmental Exposure Measurement in Molecular Epidemiology. Cancer Epidemiology Biomarkers & Prevention. 2005; 14(8): 1847–1850.
- Exposome and Exposomics. [Internet]. CDC. [cited 17 June 2020]. Available from: https://www.cdc.gov/niosh/topics/exposome/default.html
- Money CD, Gray CN, Exhaled Breath Analysis as a Measure of Workplace Exposure to Benzene ppm. The Annals of Occupational Hygiene. 1989; 33(2): 257–262.
- Brugnone F, Perbellini L, Faccini G.B,. et al. Breath and blood levels of benzene, toluene, cumene and styrene in non-occupational exposure. International Archives of Occupational and Environmental Health. 1989; 61: 303–311.
- De Lacy Costello B, Amann A, Al-Kateb H,. et al. A review of the volatiles from the healthy human body. Journal of Breath Research. 2014; 8(1).
- Pauling L, Robinson A, Teranishi R, Cary P. Quantitative Analysis of Urine Vapor and Breath by Gas-Liquid Partition Chromatography. PNAS. 1971; 68(10): 2374–2376
- Teranishi R, Mon TR, Robinson AB, Cary P, Pauling L. Gas Chromatography of Volatiles From Breath and Urine. Analytical Chemistry. 1972; 44(1): 18–20.
- EPHOR consortium [Internet]. [Cited 17 June 2020]. Available from: https://www.ephor-project.eu/