Tackling the silent pandemic: AMR Industry Alliance sets the Standard
Posted: 17 August 2022 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
Here AMR Industry Alliance representatives Melissa Gong Mitchell and Steve Brooks discuss how the Alliance is mobilising the life sciences sector in combatting antimicrobial resistance (AMR). They present the newly established antibiotics manufacturing standard that aims to minimise pharma’s contribution to AMR in the environment, considering the critical considerations and challenges companies may face when establishing effective waste management systems.


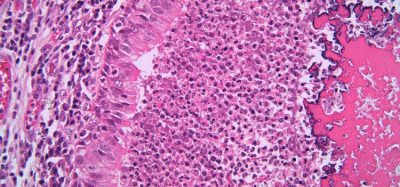
Antimicrobial resistance (AMR) is a growing concern worldwide. Recognised as one of the top 10 global health changes by the World Health Organization (WHO),1 it was found to have played a role in 4.95 million deaths in 2019 and been the direct cause of 1.27 million of these,2 meaning drug-resistant infections killed more people than HIV/AIDS (864,000 deaths) or malaria (643,000 deaths).3 Just six resistant bacteria accounted for almost 80 percent of the direct deaths, with antibiotic-resistant Escherichia coli killing around 200,000 people alone.2 While AMR is often discussed with respect to bacteria, resistance is also growing in viruses, particularly HIV, and fungi such as Candida auris.
Despite this toll, AMR has often been called the ‘silent pandemic’:4 “AMR is sadly silent because it has not been discussed like other pandemics – and of course has been in the shadow of the COVID-19 pandemic in recent years,” commented Melissa Gong Mitchell, Secretariat Lead of the AMR Industry Alliance. She attributed this to a lack of understanding of the burden of AMR, in part because many patient’s families may not know their loved one died due to an AMR related hospital infection picked up in the hospital during some other procedure.
What are the causes of AMR and how is the pharmaceutical industry implicated?
Steve Brooks, Manufacturing Lead at the AMR Industry Alliance (Advisor to the Alliance): AMR is multifaceted; there are many potential causes, including environmental ones. The main cause of antibiotic resistance is antibiotic use. When we use antibiotics, some bacteria die but resistant bacteria can survive and even multiply. The overuse of antibiotics makes resistant bacteria more common this includes overuse of antibiotics for human treatment as well as use in agriculture. Antibiotics getting into the food chain also plays a key role in the development of AMR.
On the environmental side, the issues range from lack of proper sanitation and hygiene – these are especially challenging in developing economies – all the way through to concerns about the presence of antibiotics in the environment from, for example, manufacturing. Antibiotic production is just one of many ways antibiotics can find their way into the environment.
The industry makes critical medicines, including antibiotics, that underpin the health systems of all economies, so they must be made. Antibiotic production processes involve a risk that, if operations and waste management practices are not strictly controlled, antibiotic can leave manufacturing plants in waste water, for example, and enter the environment in concentrations that may increase the risk of AMR
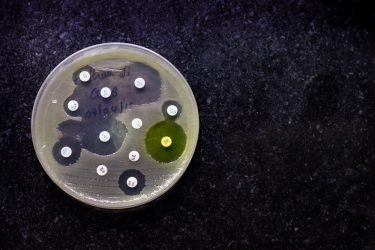
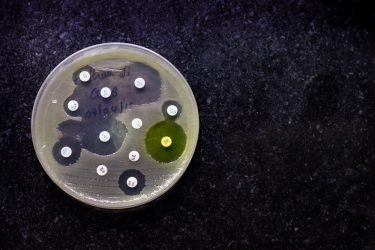
The concern is that bacteria present within the environment, say those in a water course where antibiotics are discharged, could develop resistance. Science has established that antibiotic-resistant bacteria can transfer their resistance to other bacteria through mechanisms such as horizontal gene transfer.5 If resistance is transferred to pathogenic bacteria and those find their way in sufficient quantities to humans, there is potential for an untreatable infectious disease.
About the AMR Industry Alliance
Mitchell explained: “The AMR Industry Alliance was created to be an industry voice on AMR. We are the largest life sciences coalition bringing together various life science industry representatives,” including over 100 biotech, diagnostics, generics and research-based pharmaceutical companies and associations, to drive collaborative approaches and measure the life-sciences’ industry progress to curb AMR. The Alliance was established in 2016 to ensure its signatories meet the commitments outlined in its Declaration on Combatting Antimicrobial Resistance (January 2016) and Roadmap (September 2016; updated 2019).
“We have four focus areas for projects: access, appropriate use, manufacturing, and research and science. At any point in time, we are working with industry leaders, both our members and others from governments and global institutions, on multiple projects in the fight against AMR,” added Mitchell.
What is the Antibiotic Manufacturing Standard and why was it developed?
Brooks: Currently there is no way to scientifically assess the risk to human health from the presence of antibiotics in the environment – this science is still evolving. However, the Alliance, along with many other stakeholders, recognises that while the risks cannot be quantified, there is a concern. This is why we developed a manufacturing standard; to minimise the contribution antibiotics manufacturers are making to AMR, even in the absence of any other type of control (eg, government regulation).
Our members have been implementing these requirements for some time, under the Alliance’s 2018 Common Antibiotic Manufacturing Framework, which described a risk-based approach to assessing and controlling antibiotic manufacturing waste streams, but the standard was launched to clarify that there is a specification that all antibiotic manufacturers should adopt and that stakeholders, such as large antibiotic procurers, as procurers, should be aware of. It is a proactive step by industry.
Why is wastewater a major focus of the Antibiotic Manufacturing Standard?
Brooks: Wastewater is the primary focus of the standard because not only can exposure of environmental bacteria to antibiotics potentially create and transfer resistance, but there is also a concern that the passage of waste streams through biological wastewater treatment plans, which contain bacteria, could mix antibiotics with bacteria and create resistance.


In the pharmaceutical industry, we manage solid waste streams pretty well. These steams are well regulated, especially in developed economies, so the risk from solid waste – while not zero – is less of a concern. For example, if you are treating solid waste in the US, you might incinerate it or take it to a licensed landfill site that is strictly regulated and has well controlled leachate (runoff from the landfill).
But despite pharmaceutical manufacturing operations being subject to control of traditional waste parameters in the aquatic environment, such as chemical, biological, oxygen demand and pH, there are generally no specific controls over concentrations of antibiotics that may be released.
Antibiotic manufacture often involves handling powders at some point and after transfer of those powders you need to clean production equipment and whole manufacturing suites. If that waste contains antibiotic residues and goes into your wastewater system (eg, as a result of equipment wash down), these residues are likely to be released into the environment in receiving water (such as a river) because typical wastewater treatments may not remove all antibiotic residues. Removal is dependent on the type of treatment you have.
Our standard focuses more on wastewater because solid waste and air emissions are less likely to contribute to AMR. However, we do require proper control of solid waste in the standard, as well as proper storage of antibiotics and antibiotic waste to prevent leakage, which could otherwise enter the wastewater system.
What are the key considerations when establishing effective waste management systems?
Brooks: From the Alliance perspective, leadership commitment to establishing long-term goals to reduce concentrations of residual antibiotics from manufacturing to levels unlikely to cause harm in the environment was critical, as without this it would have been difficult to make progress. The standard has two key requirements at an antibiotic manufacturing site:
- The presence of an effective environmental management system to identify and minimize possible antibiotic emissions
- The antibiotic concentration in manufacturing wastewater discharge is safe, ie, unlikely to increase the risk of AMR developing in environmental bacteria.
The standard outlines an approach you can take to establish effective waste management systems. It has several steps:
- assessment of risk
- understanding your manufacturing process
- assessing where waste streams might contain antibiotics
- determining what concentrations of antibiotics are in those waste streams
- calculating, through mass balance, how much antibiotic is being released from your manufacturing facility and what the concentration in the receiving environment may be
- ultimately working backwards, so if you calculate that you may be releasing more than the safe target into the environment you can identify where the waste is coming from and thus how to reduce it.
One of the most important things is having access to knowledge; the standard has lots of examples of how contributions to antibiotic waste can be reduced. In establishing our standard, we pooled our collective scientific expertise and relevant antibiotic ecotoxic data across the companies – this was the first time companies had shared this kind of scientific data on their antibiotics. By pooling that information, we were able to set meaningful limits for safe concentrations of antibiotics in the environment.
The Alliance has significant experience within this area and we are willing to share our knowledge and experience, not just with our members but with other companies that are not part of the Alliance.
We also published our approach to establishing safe methods in scientific literature, including the safe limits themselves for about 120 antibiotics.6
What challenges may companies encounter when setting up compliant waste management systems?
Brooks: There are several potential challenges; the first is commitment. You must be open to the issue and committed to addressing any challenges that you encounter. The standard starts with your own facility; however, for our members, we also require that their suppliers are compliant with the standard, which can be a challenge if the supplier does not understand the issue or is not committed to addressing gaps that might be found once assessments have been done.
Our standard focuses more on wastewater because solid waste and air emissions are less likely to contribute to AMR. However, we do require proper control of solid waste in the standard”
Commitment is the first piece of the puzzle, but technical knowledge is the second. A proper assessment and quantification of waste requires a level of understanding of the processes and the ability to calculate mass balance – measuring and assessing all the inputs and outputs of a system and identifying what went to waste. That can be challenging without expertise.
Finally, if your waste stream does not meet the safe level or predicted no effect concentration (PNEC), and rectifying the issue requires more technical interventions, such as improving or implementing additional wastewater treatment technology, then this can be challenging.
However, none of these issues are insurmountable. Ultimately, I believe the work we are doing is proportionate to the risk and that it is pragmatic. In other words, it can be done – we have evidence of this through our members.
Beyond manufacturing, what is the AMR Industry Alliance focused on?
Mitchell: We are constantly working on numerous initiatives across our various areas of focus. We are looking at two areas in the access space:
- scaling access to the right antibiotics at the right time in hospital settings for low- and middle-income countries (LMICs), developing a practical implementation guide for hospital administrators on the access and appropriate use of antimicrobial drugs and diagnostics
- sustainable off-patent antibiotics supply – developing policy recommendations that can help overcome global challenges for antibiotics access.
In the appropriate-use space, we are also focused on two specific areas: stewardship, with our Stewardship Prize recognising best practices and good stewardship in ongoing programmes globally; and the role of diagnostics to overcome inappropriate use of antimicrobials.
AMR is sadly silent because it has not been discussed like other pandemics – and of course has been in the shadow of the COVID-19 pandemic in recent years”
In our research and science space, the Alliance recently supported a new report researched and authored by One Health Trust, which identifies key regulatory challenges that are associated with AMR innovation and research in three key countries – South Africa, India and Brazil.7 We want to improve the convergence of the regulatory environment to ensure that innovation, research, clinical trials and commercialisation can happen and regulatory-based incentives are in place.
Overall, our goal with the Alliance is to align this cross-sector life sciences group on the important topic of combatting AMR. We always welcome others to join the conversation, be part of the Alliance and get engaged in our projects.
About the author
Hannah Balfour is the Science Writer for European Pharmaceutical Review.
References
- Antimicrobial resistance [Internet]. Who.int. 2022 [cited 1 July 2022]. Available from: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- Murray C, Ikuta K, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet. 2022;399(10325):629-655.
- Thompson T. The staggering death toll of drug-resistant bacteria. Nature. 2022;. DOI: https://doi.org/10.1038/d41586-022-00228-x
- Dodson K. Antimicrobial Resistance is the silent pandemic we can no longer neglect [Internet]. unfoundation.org. 2021 [cited 6 July 2022]. Available from: https://unfoundation.org/blog/post/antimicrobial-resistance-is-the-silent-pandemic-we-can-no-longer-neglect/
- Sun D, Jeannot K, Xiao Y, Knapp C. Editorial: Horizontal Gene Transfer Mediated Bacterial Antibiotic Resistance. Frontiers in Microbiology. 2019;10.
- Tell J, Caldwell D, Häner A, et al. Science‐based Targets for Antibiotics in Receiving Waters from Pharmaceutical Manufacturing Operations. Integrated Environmental Assessment and Management. 2019;15(3):312-319.
- Kalanxhi E, Parameswaran G, Van Wijk M, et al. Drug Regulatory Approvals and Opportunities for Antimicrobial Innovation – Perspectives from Brazil, India and South Africa [Internet]. Washington DC: One Health Trust; 2022. Available from: https://www.amrindustryalliance.org/…
Related topics
Antibiotics, Drug Manufacturing, Environmental Monitoring, Good Manufacturing Practice (GMP), Industry Insight, Microbiology, Regulation & Legislation, Therapeutics
Related organisations
Related drugs
Related diseases & conditions
AIDS, Antibiotic resistance, bacterial infections, HIV (Human Immunodeficiency Virus), Malaria