Implementing global standards to ensure end‑to‑end FMD compliance
Posted: 1 July 2019 | Neil Piper | No comments yet
Effective drug serialisation and identification is essential for improving the safety of medicines and combatting counterfeits. The Falsified Medicines Directive’s new requirements promise to crack down on the impacts of unsafe drugs. Neil Piper discusses the human cost of falsified medicines and how companies need to increase traceability of individual drug packets going forward.
The global impact of falsified medicines


The World Health Organization (WHO) references unlawful medications as substandard and falsified (SF) medical products. WHO further defines falsified medicines as “medical products that deliberately/fraudulently misrepresent their identity, composition or source.”1 According to WHO, approximately one in 10 pharmaceutical products in low- and middle-income countries are either substandard or falsified.2 As of November 2017, they reported that “twenty global medical product alerts and numerous regional warnings” had been issued, with “technical support provided in more than 100 cases.”2
Accounting for compounding factors such as the impact of loss of income to pharmaceutical companies and governments, as well as remedial expenses, it has been estimated that the cost to the European Commission equates to €950m per year.3 By 2020, it is predicted that the falsified market in Europe could be worth €3.3bn,4 highlighting the sheer scale of the problem. The financial consequences are real, but the most compelling and worrying implications arise when considering the severe level of risk to human health.
The human cost
Annually, hundreds of thousands of children in lower-income countries die as a direct result of having consumed drugs for treating malaria, pneumonia and other diseases that are either substandard or falsified.5 However, high-income countries aren’t immune from the challenges of counterfeit medicines. Perhaps the most prominent news story in recent months has been the identification of a counterfeit form of the drug Xanax, which is reported to have claimed more than 200 lives in the UK and 126 in Scotland alone.6
How could standards help?
Maintaining and enhancing the integrity of the end-to-end pharmaceutical supply chain is vital to help prevent the infiltration of falsified medicines. The introduction of a standardised, unique identification system for drugs or medical devices will enable the authentication and traceability of products. This would help to combat the ability of counterfeiters to integrate their products into the healthcare supply chain. Adopting a single, global standard in healthcare would provide key supply chain stakeholders with complete visibility and the ability to track products from manufacturer to patient. The benefits would include critical patient safety and cost savings. A recent McKinsey study7 highlighted just how important standards are:
- Implementing global standards across the entire healthcare supply chain could save 22,000–43,000 lives and avert 0.7 to 1.4 million patient disabilities
- Rolling out standards-based systems globally could prevent tens of billions of dollars’ worth of counterfeit drugs from entering the legitimate supply chain
- Healthcare costs could be reduced by $40‑$100bn globally by the implementation of global standards.
International organisations are working collaboratively to prevent counterfeits from reaching the patients. For example, Interpol Foundation, WHO and the World Customs Organization are working alongside regulators such as the US Food and Drug Administration (FDA) and the EU Commission. Collectively, they are working to raise global awareness, introducing sanctions and introducing measures to secure the supply chain.
The Falsified Medicines Directive


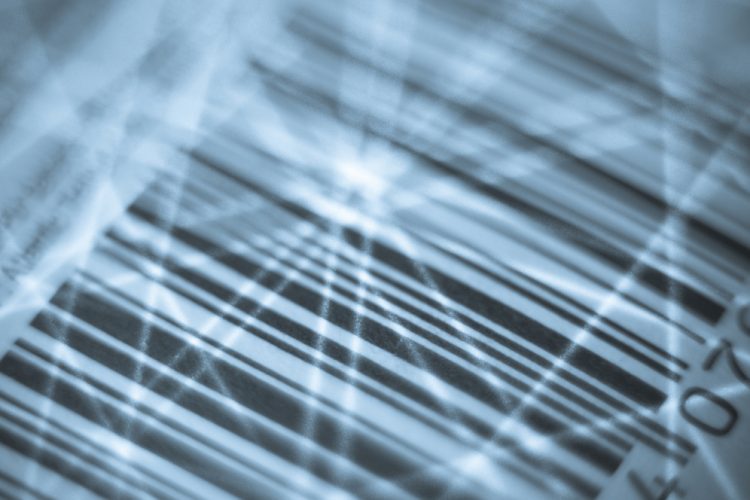
The FMD integration is compulsory for any company selling or buying drugs – failure to comply means that pharmaceutical companies cannot sell their products. The directive requires the serialisation of prescribed drugs; every pack can be verified and decommissioned. If anything needs recalling, it can be identified down to the individual packet – a radical change for pharmacies and for manufacturers.
All medicinal products for human use need to have and adhere to two key safety feature requirements. The first supports the use of a single global standard, validating the comments in the McKinsey report. The second is the implementation of an anti-tampering device on a product’s packaging. In accordance with the first principle, each product package is required to carry a unique identifier,8 “a unique sequence carried by a two-dimensional barcode allowing the identification and authentication of the individual pack on which it is printed.”
What next for pharmaceutical manufacturers?
Pharmaceutical manufacturers need to consider and invest in technology that can cope with significantly different requirements from global organisations. They need to be able to report into different regulatory databases, which may have varying requirements of data to be updated at various points in the supply chain.
pharmaceutical manufacturers need to consider and invest in technology that can cope with significantly different requirements from global organisations
With every medicine receiving a different serial number, systems are needed to manage and track information related to the product and its movement. Systems infrastructure will need to be able to condense data from vast networks and upload all information to a national or European database. Each manufacturer should also ensure they have aggregation solutions in place to allow for a full track-and-trace model, as this could potentially become a requirement in Europe.
Despite the considerations and investment that must be made by pharmaceutical manufacturers, serialisation and the use of standards provide opportunities for the future. These have already been validated and are in use in the retail sector, with very tangible benefits.
Serialisation in the UK
Serialisation in the UK’s NHS system would have unprecedented benefits, particularly in acute trust settings to create a safer and more efficient service. Medications need to be tracked and traced throughout the patient pathway with ease, even to patient application. There are tangible benefits and cost savings in operational efficiencies such as the ability to automatically validate expiry dates, preventing the use or sale of expired medicines.
Identifying every product empowers healthcare professionals by allowing them to easily access accurate and transparent product information, facilitating precise ordering, improving product availability and lowering transaction costs. However, the real power comes in the ability to effortlessly identify and remove all recalled products across trusts, down to the patient level, once they have been discharged.
Conclusion
As the development of falsified medicines becomes increasingly sophisticated, the healthcare system needs to constantly evolve to ensure it has robust processes in place to reinforce the supply chain.
Global efforts are being made to transform the pharmaceutical supply chain, increasing visibility and traceability throughout. Ultimately, the aim is to reduce the risk of harm to patients. To achieve this, standards need to prove their critical worth in ensuring a seamless, lean and secure end-to-end distribution practice.
Biography
NEIL PIPER is an Auto ID expert and business consultant, with over 25 years’ experience working predominantly in the Retail and Healthcare sectors. Skilled in GS1, ISBT standards, barcode technologies (printing and scanning), RFID, EPCIS, regulatory compliance (FMD, UDI both FDA and EU MDR/IVDR, UK MHRA GS1 compliance and more). He is currently redrafting ISB 1077 and ISB 0108 standards to comply with NHS Digital requirements. He has provided consultancy to numerous NHS trusts, pharmaceutical and medical device suppliers.
References
- Health Organization. (2019). Definitions of Substandard and Falsified (SF) Medical Products. [online] Available at: https://www.who.int/medicines/regulation/ssffc/definitions/en/ [Accessed 4 Jun. 2019].
- int. (2019). Substandard and falsified medical products. [online] Available at: https://www.who.int/news-room/fact-sheets/detail/substandard-and-falsified-medical-products [Accessed 4 Jun. 2019].
- europa.eu. (2019). [online] Available at: https://ec.europa.eu/health/sites/health/files/files/pharmacos/pharmpack_12_2008/counterfeit-ia_en.pdf [Accessed 4 Jun. 2019].
- eu. (2013). [online] Available at: https://eaasm.eu/public/downloads/3wxmE/Falsified+Medicines+costing+the+earth-2.pdf [Accessed 4 Jun. 2019].
- BBC News. (2019). ‘Xanax’ linked to more than 200 deaths. [online] Available at: https://www.bbc.co.uk/news/health-47055499 [Accessed 4 Jun. 2019].
- Susan Scutti, C. (2019). Global ‘pandemic’ of fake drugs killing children worldwide. [online] CNN. Available at: https://www.cnn.com/2019/03/11/health/fake-drugs-killing-children-study/index.html [Accessed 4 Jun. 2019].
- org. (2012). [online] Available at: https://www.gs1.org/docs/healthcare/McKinsey_Healthcare_Report_Strength_in_Unity.pdf [Accessed 4 Jun. 2019].
- europa.eu. (2019). [online] Available at: https://ec.europa.eu/health/sites/health/files/files/falsified_medicines/qa_safetyfeature_en.pdf [Accessed 4 Jun. 2019].
Issue
Related topics
Drug Counterfeiting, Drug Safety, Packaging, QA/QC, Regulation & Legislation