Cilta-cel induces deep and durable responses in relapsed or refractory multiple myeloma trial
Posted: 2 June 2021 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
New trial data shows 98 percent of heavily pre-treated relapsed/refractory multiple myeloma patients responded to Janssen’s ciltacabtagene autoleucel (cilta-cel).
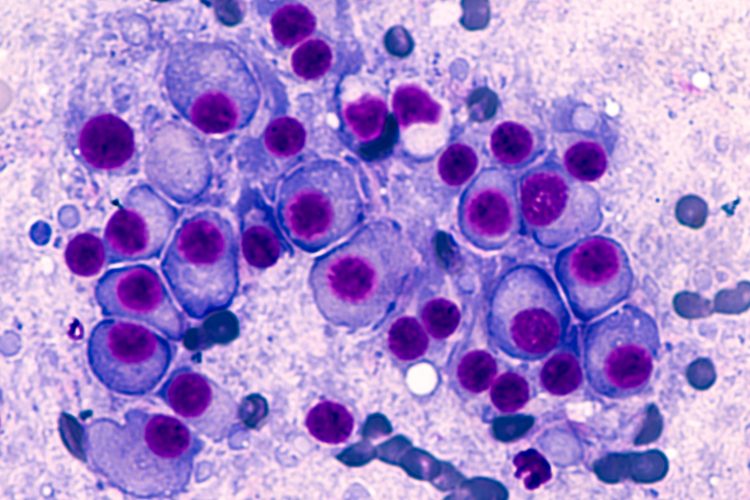
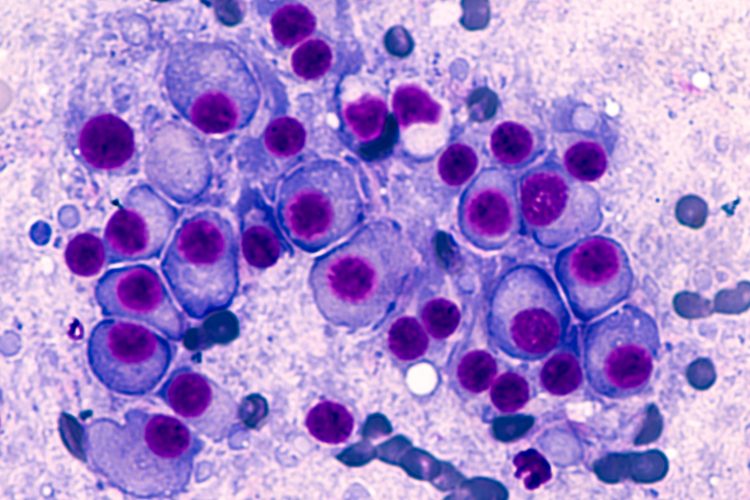
Bone marrow aspirate cytology of multiple myeloma, a type of bone marrow cancer of malignant plasma cells, associated with bone pain, bone fractures and anemia.
The Janssen Pharmaceutical Companies of Johnson & Johnson have released new data for ciltacabtagene autoleucel (cilta-cel), an investigational B-cell maturation antigen (BCMA)-directed chimeric antigen receptor (CAR)-T therapy. Updated results from the Phase Ib/II CARTITUDE-1 study show 98 percent of patients with heavily pre-treated relapsed/refractory multiple myeloma (RRMM) responded to treatment with cilta-cel and 80 percent achieved a stringent complete response (sCR) at a median follow-up of 18 months.
In addition to the response to treatment deepening over time (the previous overall response rate [ORR] was reportedly 67 percent), 66 percent of patients were progression free and alive at 18 months and the overall survival (OS) was 81 percent. The findings will be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting.
“The efficacy results observed in heavily pre-treated patients with multiple myeloma receiving cilta-cel are remarkable,” said Dr Saad Usmani, Division Chief of Plasma Cell Disorders, Levine Cancer Institute, US, and principal study investigator. “With the possibility of achieving the progression-free survival reported and responses deepening as observed in the longer-term follow-up, I am hopeful that cilta-cel will be part of the armamentarium in the future for patients in need of an additional treatment option.”
The study (NCT03548207) included patients who had received a median of six prior treatment regimens (range: three to 18). All patients were triple-class [immunomodulatory agent (IMiD), a proteasome inhibitor (PI) and an anti-CD38 antibody] exposed, while 42 percent of patients were penta-drug refractory and 99 percent of patients were refractory to the last line of therapy. Overall, 14 percent of patients achieved a very good partial response (VGPR) and three percent achieved a partial response (PR). Median time to first response was one month and responses deepened over time. Among 61 minimal residual disease (MRD) evaluable patients, 92 percent of patients achieved MRD negativity status at 10-5 at a median of one month post infusion.
The data demonstrated a consistent safety profile for cilta-cel and no new safety signals were observed with longer follow-up. The most common haematologic adverse events (AEs) observed in the CARTITUDE-1 study were neutropenia (96 percent); anaemia (81 percent); thrombocytopenia (79 percent); leukopenia (62 percent); and lymphopenia (53 percent). Cytokine release syndrome (CRS) of any grade was observed in 95 percent of patients with a median duration of four days and 99 percent of which resolved within 14 days of onset. Of the 92 patients with CRS, 95 percent experienced Grade 1/2 events. Neurotoxicity of any grade was observed in 21 percent of patients, with Grade 3 or higher neurotoxicity observed in 10 percent.
Data from the CARTITUDE-1 study supported the US Food and Drug Administration (FDA) Biologics License Application, which has recently been accepted for priority review.
Related topics
Anti-Cancer Therapeutics, Biologics, Clinical Trials, Drug Development, Drug Safety, Immunotherapy, Research & Development (R&D), Therapeutics
Related organisations
Janssen Pharmaceutical Companies of Johnson & Johnson, Levine Cancer Institute









