Pharmacovigilance Risk Assessment Committee (PRAC) meeting highlights, March 2022
Posted: 14 March 2022 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
EMA’s pharmacovigilance committee recommends product information updates for two COVID-19 vaccines – Janssen COVID-19 Vaccine and Moderna’s Spikevax.


In its latest meeting the European Medicines Agency (EMA) Pharmacovigilance Risk Assessment Committee (PRAC) recommended adding small vessel vasculitis as a side effect to the Janssen COVID-19 Vaccine product information, among other activities.
Janssen COVID-19 Vaccine: small vessel vasculitis now a side effect
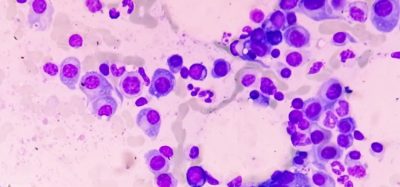
PRAC has recommended that small vessel vasculitis with cutaneous manifestations (inflammation of blood vessels in the skin which may result in a rash, pointed or flat, red spots under the skin’s surface and bruising) should be added to the product information of Janssen COVID-19 Vaccine as a possible side effect of unknown frequency.
Small vessel vasculitis can be caused by viral or bacterial infections as well as by medicines and vaccines. Generally, manifestations of the disease spontaneously resolve over time with appropriate supportive care.
The decision was based on a review of 21 cases reported globally, including 10 cases consistent with the established definition of single organ cutaneous vasculitis (vasculitis affecting a single organ). For most of these 10 cases no other obvious explanation was identified; eight of these cases occurred soon after the administration of the vaccine.
As of 31 December 2021, approximately 42.5 million doses of the vaccine had been administered worldwide. PRAC will continue to monitor further cases of vasculitis and communicate if new information becomes available.
EMA's safety committee recommends updates to product information for COVID-19 Vaccine Janssen to include a new possible side effect and for Spikevax to include a new warning for flare-ups of capillary leak syndrome. #PRAC #COVID19vaccines #SafetyOfVaccines https://t.co/AE50NiN11m pic.twitter.com/yDA6FtfLXO
— EU Medicines Agency (@EMA_News) March 11, 2022
Warning of capillary leak syndrome with Spikevax
The committee recommended adding a warning about flare-ups of capillary leak syndrome (CLS) to the product information for Spikevax, Moderna’s COVID-19 vaccine.
CLS is an extremely rare, serious condition that causes fluid leakage from capillaries, resulting in rapid swelling of the arms and legs, sudden weight gain, feeling faint, thickening of the blood, low blood levels of albumin and low blood pressure. CLS is frequently related to viral infections, some blood cancers, inflammatory diseases and some treatments.
In making the recommendation, PRAC accessed all available Eudravigilance data on CLS cases reported after the administration of the mRNA vaccines Spikevax and Comirnaty. The committee concluded there was “insufficient evidence to establish a causal association between the two vaccines and the onset of new cases of CLS”. They did however recommend that a warning about CLS be added to Spikevax’s product information to raise awareness of the potential risk of flare-ups among healthcare professionals and patients, “as some cases of flare-ups of CLS pointed towards an association with Spikevax, while the cases reported after vaccination with Comirnaty did not support such association”.
Healthcare professionals should be aware of the signs and symptoms of CLS and of a possible risk of flare-ups in people with a history of CLS. Vaccinated individuals with a history of CLS should consult their treating physician when planning their vaccination.
In total 55 reported cases of CLS were reviewed, 11 with Spikevax and 44 with Comirnaty. Global exposure at the time of the assessment was estimated at approximately 559 million doses for Spikevax and 2 billion doses for Comirnaty.
Direct healthcare professional communication (DHPC) for dexmedetomidine
In the meeting, PRAC discussed a direct healthcare professional communication (DHPC) aimed at informing healthcare professionals that there is an increased risk of mortality when administering dexmedetomidine in intensive care unit (ICU) patients aged 65 years and less, compared with alternative sedatives.
Dexmedetomidine is a medicine authorised for light sedation of adult patients in ICUs.
The SPICE III study was a randomised clinical trial comparing the effect of sedation with dexmedetomidine on all-cause mortality to that of usual standard of care in 3,904 critically ill adult ICU patients in need of mechanical ventilation. The study showed no difference in the overall 90-day mortality between dexmedetomidine and alternative sedatives (Propofol, midazolam); however, dexmedetomidine was associated with an increased risk of mortality in patients aged 65 years and less.
The product information for dexmedetomidine is being updated with a warning describing the evidence and risk factors. Healthcare professionals are being advised to weigh these findings against the expected clinical benefit of dexmedetomidine compared to alternative sedatives in this age group.
The DHPC for dexmedetomidine will be forwarded to EMA’s human medicines committee, Committee for Medicinal Products for Human Use (CHMP) for approval before being disseminated to healthcare professionals by the marketing authorisation holder and published on the Direct healthcare professional communications page and in national registers in EU Member States.
Related topics
Biologics, Clinical Trials, Drug Safety, Regulation & Legislation, Vaccines
Related organisations
EMA Pharmacovigilance Risk Assessment Committee (PRAC), Janssen Pharmaceutical Companies of Johnson & Johnson, Moderna, The European Medicines Agency (EMA)