Cancer immunotherapy drugs linked to autoimmune diseases
Posted: 24 June 2016 | | No comments yet
Some cancer patients taking the immunotherapy drugs ipilimumab and nivolumab may be at a higher-than-normal risk of developing autoimmune diseases…


Johns Hopkins Medicine researchers have reported that a small number of cancer patients taking the immunotherapy drugs ipilimumab and nivolumab may be at some higher-than-normal risk of developing autoimmune joint and tissue diseases, including inflammatory arthritis.


“I don’t think anyone is particularly surprised that rheumatologic disorders might be a complication of drugs that boost the immune system,” says Laura C. Cappelli, M.D., a rheumatologist at the Johns Hopkins University School of Medicine. But the preliminary study, however small in sample size, she says, is believed to be the largest published case series of a link between the immunotherapy drugs and the diseases.
The patients described in the new case report make up only about 1.3 percent of the total patients treated with drugs – singly or in combination – at The Johns Hopkins Hospital from 2012 to 2016, Cappelli says, but if further research confirms a cause-and-effect relationship, the rate is likely an underestimation of how common rheumatologic diseases are in patients taking immune checkpoint inhibitors. She notes that patients with only mild joint pain, for instance, or those with already deteriorating health from their cancers may not have been referred to the rheumatology clinic for their symptoms.
“We keep having referrals coming in from our oncologists as more patients are treated with these drugs,” says Clifton Bingham, M.D., associate professor of medicine at the Johns Hopkins University School of Medicine and director of the Johns Hopkins Arthritis Centre. “In particular, as more patients are treated with combinations of multiple immunotherapies, we expect the rate to go up.”
13 patients developed new-onset arthritis or sicca syndrome
Between 2012 and 2016, 13 patients at the Johns Hopkins Kimmel Cancer Centre who were taking one or both immunotherapy drugs to treat their cancers developed new-onset arthritis or sicca syndrome.
“In 2015, our rheumatology clinic started getting more and more referrals from our oncology department to evaluate patients treated with immunotherapies,” says Cappelli. “And the patients we saw had very severe, highly inflammatory arthritis. They needed even higher doses of steroids to control their symptoms compared to what is needed in other forms of inflammatory arthritis, like rheumatoid arthritis.”
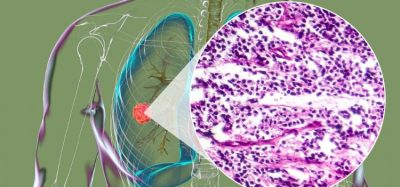
Ipilimumab and nivolumab are designed to turn off the molecular checkpoints that some cancers use to evade the body’s natural immune system cells. The allow the immune system to detect and attack tumour cells. But because they also turn up the activity of the immune system as a whole, the drugs can trigger immune-related side effects, including autoimmune responses.
Cappelli notes that clinical trials of ipilimumab and nivolumab found an increased risk of inflammatory bowel diseases, lung inflammation, autoimmune thyroid disease and pituitary gland inflammation. But those trials were designed primarily to determine efficacy against cancer and not to fully examine all features of rheumatologic side effects, she says.
Cappelli says she wants the case report to raise awareness among both patients and clinicians that rheumatologic side effects may occur with the drugs. “It is important when weighing the risk-benefit ratio of prescribing these drugs,” she says. “And it’s important for people to be on the lookout for symptoms so they can see a rheumatologist early in an effort to prevent or limit joint damage.”