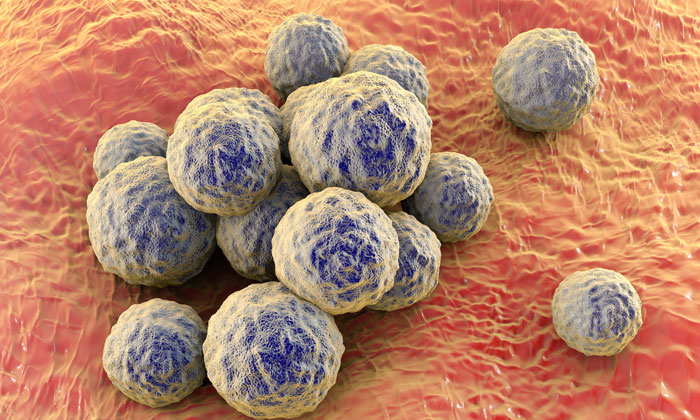
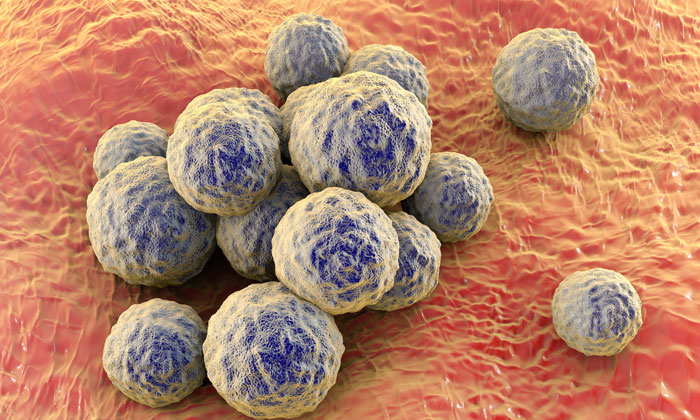
Treatment for MRSA no longer more costly than for susceptible Staph aureus infections
Posted: 11 May 2018 | European Pharmaceutical Review | No comments yet
A new study found that infections caused by the drug resistant bacteria – methicillin-resistant Staphylococcus aureus, known as MRSA – are no more expensive to treat than MSSA, the methicillin-susceptible version of the same bacteria.
These findings, from researchers at the Center for Disease Dynamics, Economics & Policy (CDDEP), with collaborators from Johns Hopkins University and University of Texas Southwestern Medical Center, are contrary to earlier studies that have found that MRSA was much more expensive to treat than MSSA.
The researchers used national hospitalisation data to analyse the costs of treating patients diagnosed with S. aureus infections from 2010 to 2014. Costs were assessed in aggregate and by three infection types: S. aureus blood stream infections, S. aureuspneumonia infections, and other S. aureus infections, primarily skin and soft tissue infections. Surprisingly, MSSA infections were found to be costlier than MRSA infections across all infection types. However, after controlling for differences in the patient populations infected with MRSA and MSSA, only skin and soft tissue MSSA infections were estimated to be costlier – while for other infection sites the costs were similar.
“Contrary to historical studies at the hospital-level, which suggested that MRSA infections were significantly more expensive that MSSA infections, nationally we found that MRSA-related hospitalisation costs were approximately the same as or less expensive than hospitalisations with MSSA infections,” according to the study’s lead author Dr. Eili Klein, Research Fellow at CDDEP.
However, researchers noted that patients with MRSA infections had a greater likelihood of mortality than patients with MSSA.
One potential reason for the convergence in costs of treating MSSA and MRSA is the emergence and spread of community-associated strains of MRSA. These strains, which are genetically distinct from hospital-associated strains and have different infection patterns and antibiotic susceptibilities, surged in the early 2000s. This may have led physicians to empirically treat all potential S. aureus infections as if they were MRSA, which may have improved outcomes and costs for treating infected MRSA patients while increasing costs for treatment of MSSA patients.
The study was unable to determine if the change was a function of improved diagnostic tests, better empiric prescribing, or changes in hospital infection control. “Changes in the health insurance system may have also affected hospital care and treatment costs,” continued Dr. Klein. “Further research is needed to better understand the underlying reasons for the change and the implications of this research for the broader crisis of antibiotic resistance.”
Related topics
Related organisations
Center for Disease Dynamics, Economics & Policy (CDDEP), Johns Hopkins University, University of Texas Southwestern Medical Center








