Genetically modified viral injection could treat metastatic melanoma
Posted: 28 January 2019 | European Pharmaceutical Review | No comments yet
A study has reported that almost 40 percent of patients with non-surgically treatable tumours were effectively treated using a genetically modified virus…
The injection of a genetically modified virus that induces the body’s own immune cells to attack metastatic melanoma effectively treated almost 40 percent of patients with tumours that could not be surgically removed.
“Our findings in the real world mimic what the clinical trials have found,” said corresponding author Dr David W. Ollila, a general surgical oncologist, department of surgery, University of North Carolina at Chapel Hill. “It’s a different world now in metastatic melanoma, because instead of the traditional cytotoxic chemotherapy that not only kills cancer cells but also kills normal cells, we’re stimulating the immune system to attack the cancer cells.”
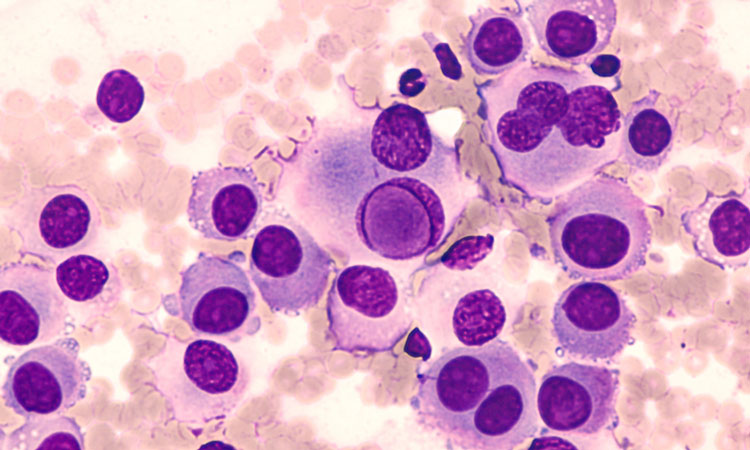
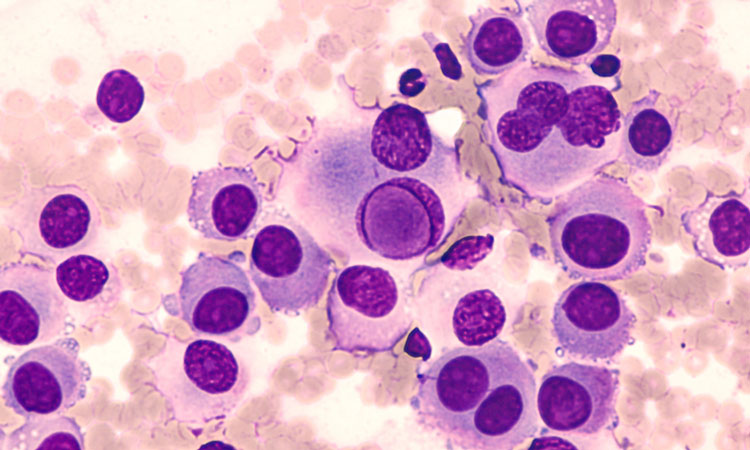
The researchers evaluated 80 adult patients treated with talimogene laherparepvec (TVEC, sold under the brand name Imlygic, by AMGEN) over a three-year period ending in October 2018. The Food and Drug Administration approved TVEC in 2015 for the treatment of stage IIIB to advanced-stage IV metastatic melanoma. TVEC is a genetically modified herpes virus that contains the stimulatory factor known as GM-CSF that increases a tumour-specific immune response.
TVEC is injected directly into the skin tumour in the physician’s office or clinic and the patient may leave immediately afterward, without the severe side effects of chemotherapy or other cancer drugs that act on the body’s immune system. The stimulatory factor sends a signal to attract white blood cells into the tumour, Dr Ollila explained, thereby inducing the body’s activated immune system to kill the metastatic melanoma cells.
The researchers reported that 46 percent of participants (37 patients) had stage IIIB disease, 31 percent (25 patients) had stage IIIC disease, 1 percent (1 patient) had clinical stage IIID disease, and 20 percent (16 patients) had cancer that spread to a distant site at the time of treatment. Patients received a median of five cycles of TVEC. Most study patients (57 percent) received some form of therapy before enrollment in the study.
The researchers found that 39 percent of participants (31 patients) had a complete local response to TVEC therapy, and 18 percent (14 patients) had a partial response.
“It’s pretty hard to ignore a response rate of 39 percent,” Dr Ollila said. He noted that patients with stage IIIB disease had an even higher complete local response rate of 68 percent, compared with those with higher-stage disease: 26 percent for IIIC, 0 percent for IIID, and 6 percent for IV. At a median follow-up of 12 months, 59 percent of patients with stage IIIB disease showed no signs of recurrent disease.
Dr Ollila noted that these findings surpass those from the clinical trial that led to the approval of TVEC. The overall response rate from the clinical trial was 26.4 percent. However, that trial included a higher percentage of patients with cancer that had spread to other organs, including the lungs.
TVEC was also well tolerated by the study patients, Dr Ollila said. Side effects were mild and self-limited; the most common side effects were flu-like symptoms in 28 percent of participants (22 patients), whereas the side effects of chemotherapy and other drugs that activate the body’s immune system can be severe, including nausea or vomiting and immune-related toxicities. Only five patients stopped treatment for a variety of complications, including cold sores or infection.
One key takeaway from the study was that patients with stage IIIB/C or stage M1A metastatic melanoma may benefit more from the drug than those with higher stage cancers, Dr Ollila said. “We reported a complete response rate that was higher than the 2015 clinical trial because the clinical trial included higher-risk patients in whom TVEC may have limited effectiveness,” he said.
These study results raise the question of administering TVEC with other anti-cancer treatments, including drugs that inhibit the growth of other types of skin cancer cells.
“Can we now use TVEC in combination with these drugs and drive the response rates even higher?” Dr Ollila said. “Could the same principle work in metastatic merkel cell and locally advanced squamous cell carcinoma?” The latter is the focus of an ongoing clinical trial in which Dr Ollila and his co-authors are participating.
Besides chemotherapy, another existing treatment for skin cancer is surgical removal of the tumour, but that too can be problematic, Dr Ollila said. “We know that surgeons will eventually reach a point where surgical resection is no longer feasible.” The most compelling finding of the study is that it supports TVEC injection as an option for melanoma. “It appears that there’s no role for traditional chemotherapy any longer for treating this disease,” Dr Ollila added.
The study results were published in the Journal of the American College of Surgeons.
Related topics
Clinical Trials, Drug Development, Research & Development (R&D)