Bacterial Endotoxin Test using LAL methodology: overcoming interfering factors
Posted: 26 August 2021 | Tim Sandle (Bio Products Laboratory) | No comments yet
The Bacterial Endotoxin Test, using LAL methodology, is a key in-process and final product release test for sterile pharmaceuticals and medical devices. One of the challenges with LAL methodology is overcoming interfering substances as demonstrated by inhibition or enhancement of an endotoxin challenge. Here, Bio Products Laboratory’s Dr Tim Sandle discusses the interfering substances issue and provides some guidance to overcome it.
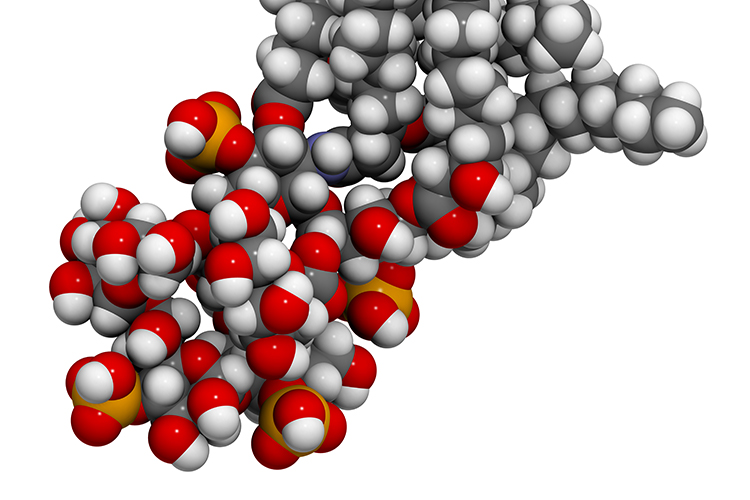
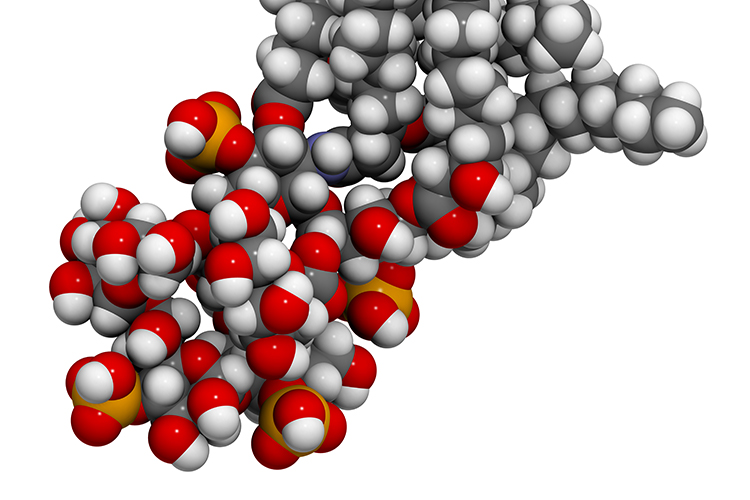
ASSESSING ENDOTOXIN levels in pharmaceutical drugs and medical devices is necessary to avoid pyrogenic response and septic shock in patients receiving these treatments. Hence, the need to perform tests for endotoxins for injectable products and medical devices is well established. The effects of endotoxin in the human body include high fever, vasodilatation, diarrhoea and foetal shock syndrome. Hence, the importance of end product testing. The Bacterial Endotoxin Test (BET) has been a pharmacopoeia method since 1980 (where it first appeared in the USP). The test, using Limulus Amoebocyte Lysate (LAL) methodology, is described in detail in the European Pharmacopoeia (Ph. Eur., 2.6.14) and US Pharmacopoeia (USP, <85>). The test describes the detection of the most common and significant pyrogenic material found in pharmaceutical production: Gram-negative bacterial endotoxin.1 The main variations between the European and US approaches relate to the acceptability of recombinant lysate and the extent of the validation required.
ASSESSING ENDOTOXIN levels in pharmaceutical drugs and medical devices is necessary to avoid pyrogenic response and septic shock in patients receiving these treatments. Hence, the need to perform tests for endotoxins for injectable products and medical devices is well established. The effects of endotoxin in the human body include high fever, vasodilatation, diarrhoea and foetal shock syndrome. Hence, the importance of end product testing. The Bacterial Endotoxin Test (BET) has been a pharmacopoeia method since 1980 (where it first appeared in the USP). The test, using Limulus Amoebocyte Lysate (LAL) methodology, is described in detail in the European Pharmacopoeia (Ph. Eur., 2.6.14) and US Pharmacopoeia (USP, <85>). The test describes the detection of the most common and significant pyrogenic material found in pharmaceutical production: Gram-negative bacterial endotoxin.1 The main variations between the European and US approaches relate to the acceptability of recombinant lysate and the extent of the validation required.
When conducting the LAL assay, it is important that the sample under test is subjected to method suitability testing. This requires setting an appropriate endotoxin limit and then challenging the sample at the appropriate dilution with endotoxin to assess for inhibition or enhancement of the challenge. This avoids under- or over-estimating the obtained result, which can occur if interfering factors are present at a significant level. This applies to both the gel-clot and photometric versions of the LAL assay, as described in the European, US and Japanese pharmacopoeia.
Inhibition and enhancement testing


For a test to be valid, it must be demonstrated that the test dilution does not exceed the maximum valid dilution and that the tested dilution does not demonstrate inhibition or enhancement of a challenge using a known concentration of endotoxin. The maximum valid dilution (MVD) is the maximum allowable dilution of a sample at which the endotoxin limit can be determined.2 The LAL reagent can be very susceptible to interference. Fortunately, the LAL test is usually more sensitive than necessary to detect the endotoxin limit for a given product or article. Inference can result from either an interaction of the sample upon the LAL reagent as well as an interaction of the sample upon the endotoxin, notably its aggregation state and availability to participate in the reaction. These interferences in the assay can influence the performance and amount of endotoxin measured by influencing the assay to under record the endotoxin (inhibition) or over record the endotoxin in the sample (enhancement).3
When performing the inhibition/enhancement, it is conducted on sample solutions at a dilution less than the MVD and one not containing any detectable endotoxins. Based on preliminary testing, the analyst should select a dilution to perform the product validation. If preliminary testing is not performed then the analyst can either validate at the MVD or make a judgement as to the dilution (not exceeding the MVD) at which they wish to validate the product. Once a non-interfering dilution has been established then the process of validation depends upon the LAL methodology being used.
Typically, validation for a finished product requires three batches to be tested for interfering factors. The test for interfering factors using the gel-clot assay requires the product to be tested against the label claim for the reagent sensitivity used. For this, a standard series is made in LAL Reagent Water (LRW) that includes 2λ, λ, ½ λ and ¼ λ in a minimum of duplicate (where λ represents the sensitivity of the lysate). A second standard series of the same concentrations is made in parallel using the product (at the non-interfering dilution or effective product treatment) as the diluent replacing LRW. This standard series must also include 2λ, λ, ½ λ and ¼ λ in a minimum of quadruplicate.
When conducting the LAL assay, it is important that the sample under test is subjected to method suitability testing”
After incubation of the assay, the endpoint gelation of the product series must have a geometric mean that is within 2λ of the geometric mean of the LRW standard series for the assay to be considered valid. Negative controls in a minimum of duplicate must also be included. This is performed on one batch of product. When the validation criteria are met, two further batches are then tested as per a routine test. The two controls must clot and the sample must not clot. All other test criteria must be met for this to be a successful validation.
The photometric assays requirement is a simpler process. Using the non-interfering dilution, or product treatment, it is necessary to test three batches of product and show that each batch of product does not exhibit interfering properties. This is performed in a minimum of duplicate and will include controls in a minimum of duplicate. If all three batches show consistent recovery of the control endotoxin within 50-200 percent then the product is validated (assuming other assay criteria are met, such as the correlation coefficient of the standard curve being greater than 0.98).
Once validated, the product should be tested under the same preparation conditions when performing the product release tests. If there are any changes to the manufacture of the product then this may affect the LAL assay and in this instance revalidation may be required.
Overcoming inhibition and enhancement
There is a range of substances that can interfere with the LAL assay, many of which are active ingredients or excipients within the formulated product.4 It is often possible to overcome interference by diluting the sample to a point at which the interfering factor ceases to affect the test, but at which the endotoxin limit concentration is still detectable. Dilution is the simplest and most widely used technique for overcoming interference – and it is effective in the majority of cases. Where this presents dilution challenges, the MVD can be overcome by changing to a more sensitive LAL reagent, varying the standard curve or changing the test method. However, it is recommended that dilution is tried before other methods of addressing interference.5
If dilution is not able to overcome the interference, then an understanding of the mechanisms of interference can sometimes help the development of an alternative strategy.6


The LAL cascade consists of a series of enzymatic reactions in which serine proteases cleave their respective substrates. The environment in which this cascade occurs affects the reaction rate and so pH and temperature are also critical to the optimum conditions of the assay. Consequently, it is important that the pH of the reaction mixture of product and LAL reagent is within the required range. While pH of the product alone could be outside the manufacturer’s stated range (usually pH 6.0-8.0), the pH of the sample and LAL together can often fall within the required range due to the buffering capacity of the LAL reagent. Similarly, the pH of the reaction mixture can be overcome by dilution. If pH problems are not overcome by dilution, then a buffer can be used to reconstitute the LAL reagent. In other cases, the sample can be diluted in buffer or adjusted by adding a solution of acid or base (HCl or NaOH). Divalent cations influence both the reactivity of endotoxin and the LAL reaction.
Divalent cations are ionic minerals such as calcium (Ca2+) and magnesium (Mg2+), which are attracted to and neutralise the negative charge of endotoxin, allowing increased aggregation size and decreasing activity/potency of the endotoxin, leading to inhibition. Dilution is the usual solution to this problem. When this cannot be overcome by dilution, endotoxin can be separated from interfering substances by ultrafiltration.
Materials that bind (chelate) divalent cations, such as EDTA (ethylene diamine tetraacetic acid) and heparin, can reduce the aggregation state of endotoxin. This results in increased reactivity, which is observed as enhancement. In contrast, sequestration of cations makes them unavailable for optimum enzyme activity of the LAL cascade, resulting in inhibition. Dilution is the best option.
Protein products or proteins in blood and blood fractions may bind endotoxin and render it unavailable for detection in the LAL test. Alternatively, some proteases degrade the proteins of the enzyme cascade while others (eg, trypsin) activate it. Heat treatment is commonly used to denature protein in a sample and allows the heat-tolerant endotoxin to be detected. Lipids and liposomes can also cause interference with the LAL test and require dissolving to overcome interference.7
Summary
Screening injectable pharmaceutical products and pharmaceutical-grade water used for product formulation for bacterial endotoxin is an important part of quality control. In doing so, it is important that the selected test dilution remains free from interfering substances (as demonstrated through inhibition and enhancement testing). This article has outlined some best practices to consider in meeting the inhibition-enhancement test challenge.
About the author
Dr Tim Sandle has over 25 years’ experience of microbiological research and biopharmaceutical processing. He is a member of several editorial boards and has authored 30 books on microbiology, healthcare and pharmaceutical sciences. Tim works for Bio Products Laboratory Limited (BPL) in the UK and is a visiting tutor at both the University of Manchester and UCL.
References
- Sandle T. (2016) Control of WFI and Clean Steam Systems for Bacterial Endotoxin. Journal of GxP Compliance, 20 (4): 1-8
- WHO (2012) Test for Bacterial Endotoxins. World QAS/11.452
- Moser K. (2009): Playing Hide and Seek with Endotoxin. LAL User Group Newsletter, 3 (2): 1-5
- Fujita Y, Nabetani T. (2014) Iron sulfate inhibits Limulus activity by induction of structural and qualitative changes in lipid A. J Appl Microbiol 116(1):89–99
- McCullogh KC, Weider-Loeven C. (1992): Variability in the LAL Test: Comparison of Three Kinetic Methods for the Testing of Pharmaceutical Products. of Parenteral Science and Technology, 46 (3): 69-72
- Barry N, Velickovic Z, Rasko J. (2020) Endotoxin quality control testing for CAR T-cell manufacturing: validation considerations for Endosafe portable testing system. Cytotherapy, 22 (5): S140,
- Roth RI, Levin FC, Levin J. (1990) Optimization of the detection of bacterial endotoxin in plasma with the limulus test. Lab. Clin. Med. 116:153-161
Issue
Related topics
Analytical techniques, Drug Safety, Endotoxin, Endotoxin Detection, Microbial Detection, Microbiology, QA/QC
Related organisations
European Pharmacopoeia (Ph. Eur.), The United States Pharmacopoeia (USP)









