Developing a holistic approach to cardio, metabolic and renal disease
Posted: 28 June 2022 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
With cardiovascular disease continuing to present a significant health concern, European Pharmaceutical Review’s Hannah Balfour reflects on recent development efforts and drug approvals in the space with comment from Dr Douglas Clark, Head of Medical Affairs at Boehringer Ingelheim UK & Ireland.


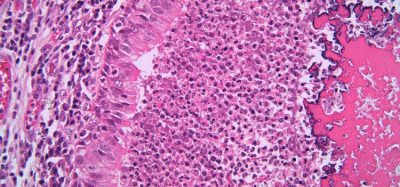
Cardiovascular diseases (CVDs) continue to present a significant health concern worldwide. According to the World Health Organization (WHO), CVDs are the leading cause of death worldwide accounting for 32 percent of global deaths in 2019 (approximately 17.9 million).1 Of these deaths, 85 percent were caused by heart attacks and strokes.
Within the UK alone, an estimated 7.6 million people are living with heart or circulatory diseases, which account for about a quarter of UK deaths each year.2 The estimated annual healthcare costs associated with circulatory disease in the UK is £9 billion.
Heart failure, a CVD in which the heart cannot effectively pump enough blood around the body, is estimated to affect approximately 920,000 people in the UK2 and more than 64 million globally.3 Heart failure with preserved ejection fraction (HFpEF) – accounting for approximately half of heart failure cases3 – has been described as the single largest unmet need in cardiovascular medicine.
To discover how the industry is responding to such critical unmet need, EPR’s Hannah Balfour discussed recent developments in the cardiology treatment field with Dr Douglas Clark, Head of Medical Affairs at Boehringer Ingelheim UK & Ireland.
Recent developments
Empagliflozin
For Boehringer Ingelheim, a critical development has been the recent regulatory approvals of empagliflozin (Jardiance®), based on results from the EMPEROR-Preserved trial.
“Empagliflozin is an oral, once daily, highly selective sodium-glucose cotransporter 2 or SGLT2 inhibitor… It was originally developed for type 2 diabetes because it improves glycaemic control,” explained Dr Clark. “Empagliflozin is indicated for adults with insufficiently controlled type 2 diabetes mellitus, but also adults with symptomatic chronic heart failure with reduced ejection fraction. In March this year, Empagliflozin was granted a Marketing Authorization by the European Commission (EC) for the treatment of adults with symptomatic chronic heart failure – expanding the existing indication of empagliflozin to include adults with HFpEF.”
Heart failure with preserved ejection fraction (HFpEF) – accounting for approximately half of heart failure cases3 – has been described as the single largest unmet need in cardiovascular medicine”
The drug was approved for the wider indication by the US Food and Drug Administration (FDA) in February 2022 and the UK’s Medicines and Healthcare products Regulatory Agency (MHRA) in June 2022.
The approvals of empagliflozin were based on data from two pivotal, placebo controlled trials – the EMPEROR-Preserved and EMPEROR-Reduced studies, involving 5,988 and 3,730 patients, respectively. In the EMPEROR-Reduced trial, 19.4 percent of patients taking empagliflozin for around 14 months were hospitalised for heart failure or died of cardiovascular causes, compared with 24.7 percent of patients taking placebo.
Of the patients taking empagliflozin for around 23 months in the EMPEROR-Preserved trial, 13.8 percent were hospitalised for heart failure or died of cardiovascular causes, compared with 17.1 for placebo.
“The pivotal Phase III studies demonstrated an improvement in the risk of cardiovascular death or hospitalisation for heart failure with empagliflozin compared to placebo in adults with heart failure with preserved ejection fraction, and in those with heart failure with reduced ejection fraction,” commented Dr Clark.
A recent real-world evidence study has added to the efficacy data, reporting that type 2 diabetes patients treated with empagliflozin were 50 percent less likely to be hospitalised for heart failure than those taking dipeptidyl peptidase-4 (DPP-4) inhibitors, and 30 percent less likely than patients taking glucagon-like peptide 1 (GLP-1) receptor agonists. Empagliflozin also reduced the relative risk of all-cause mortality by 40 percent and risk of myocardial infarction or stroke by 12 percent over DPP-4 inhibitors.
Other key regulatory decisions
In 2021, the European Medicines Agency (EMA) recommended four cardiology drugs for approval in the European Union (EU),4 including Amarin Pharmaceuticals’ Vazkepa (icosapent ethyl) to reduce the risk of cardiovascular events in patients at high cardiovascular risk, and Bayer’s Verquvo (vericiguat) for the treatment of symptomatic chronic heart failure in adult patients with reduced ejection fraction.
Two more recent approvals have come from the FDA, including the first and only small interfering RNA (siRNA) therapy to lower low-density lipoprotein cholesterol (LDL-C), Novartis’ Leqvio® (inclisiran);5 and Bristol-Myers Squibb (BMS)’s Camzyos™ (mavacamten) for adults with certain classes of symptomatic obstructive hypertrophic cardiomyopathy (HCM).6
The UK’s National Institute for Health and Care Excellence (NICE) has also recommended the use of Vazkepa® (icosapent ethyl) in adult statin-treated patients at high cardiovascular risk.7 More than one million people in England with elevated triglycerides (≥150 mg/dl [≥ 1.7 mmol/l]), LDL-C levels >1.04 mmol/l (and ≤ 2.60 mmol/l) and established CVD could benefit from the treatment on the National Health Service (NHS). Icosapent ethyl is a new active substance comprised of a highly purified omega-3 fatty acid (eicosapentaenoic acid >96 percent).
Key clinical developments
In March 2022, BMS presented interim data from an extension (EXPLORER-LTE) cohort of the MAVA-LTE study (NCT03723655) of mavacamten in HCM patients.8 In the 200+ enrolled patients, mavacamten demonstrated sustained improvements in left ventricular outflow tract gradients (LVOT-G), New York Heart Association (NYHA) Class, and N-terminal pro brain natriuretic peptide (NT-proBNP) levels – three clinically meaningful cardiovascular outcomes – at weeks 48 and 84.
Aficamten and omecamtiv mecarbil
Cytokinetics has recently presented data from the REDWOOD-HCM OLE and GALACTIC-HF trials.9 The first study showed that treatment with aficamten, an investigational selective, small-molecule cardiac myosin inhibitor, was associated with substantial reductions in the average resting LVOT-G, sustained through 24 weeks of treatment. Aficamten also improved NYHA Class in the majority of patients.9
The second trial, GALACTIC-HF, evaluated the effect of treatment with omecamtiv mecarbil in patients with heart failure with reduced ejection fraction (HFrEF) and low blood pressure. According to Cytokinetics, omecamtiv mecarbil reduced the absolute risk of cardiovascular death or heart failure events to a greater extent in patients with HFrEF and low blood pressure, than in those without low blood pressure.9
GALACTIC-HF also assessed the impact of tricuspid regurgitation (TR) on the effectiveness of omecamtiv mecarbil. Though there were more cardiovascular deaths, all-cause deaths and heart failure events in patients with moderate/severe TR, the treatment effect was consistent across patients with no TR, mild TR and moderate/severe TR, such that baseline TR did not modify the treatment effect.9
Aprocitentan
Idorsia announced that aprocitentan, a novel, oral, dual endothelin receptor antagonist (ERA), significantly reduced blood pressure when added to background antihypertensive therapy in patients with resistant hypertension.10
The PRECISION Phase III study has three parts:
- Addressing the four-week placebo-controlled efficacy of 12.5 and 25mg aprocitentan
- Assessing the durability of its effects in long-term active treatment with 25mg aprocitentan for a further 32 weeks
- A 12-week placebo-controlled withdrawal period with patients re-randomised to 25mg or placebo.
In part one, after four weeks of treatment, there was a statistically significant and clinically meaningful reduction in the primary endpoint measure of systolic blood pressure in both treatment groups, compared to placebo. In part two, the mean reduction in systolic blood pressure was maintained for patients who remained on aprocitentan, and those switching from placebo achieved the same blood pressure reduction as seen in part one. In part three, after four weeks of withdrawal, those taking placebo had significant increases in systolic blood pressure, confirming aprocitentan’s antihypertensive effect.
Future thinking: developing a holistic approach to cardio, renal and metabolic disease
Dr Clark explained that with the development of empagliflozin, as well as the company’s broader pipeline, Boehringer Ingelheim has taken an interconnected cardio, renal and metabolic disease approach.
The prevalence of comorbidity in these patients has led scientists to believe that cardio, renal and metabolic diseases may exist on a spectrum, with interconnected pathways and contributing factors”
Comorbidity is a well-established concept in the cardiovascular, renal and metabolic disease fields. A 2021 study of chronic kidney disease (CKD) found that 98.2 percent of patients with CKD had comorbidities,11 with a referenced work suggesting diabetes, obesity and hypertension were the most common.12 Furthermore, studies of diabetes patients have established the high prevalence of CVD comorbidities, a study of almost 250,000 diabetes patients found almost a third had established CVD,13 where another much larger literature review found CVD affected 32.2 of type 2 diabetes patients overall and was the cause of death for 10 percent of type 2 diabetes patients.14
The prevalence of comorbidity in these patients has led scientists to believe that cardio, renal and metabolic diseases may exist on a spectrum, with interconnected pathways and contributing factors. This theory has been supported by the clinical results of drugs such as empagliflozin, the SGLT2 inhibitor, across several of these conditions.
Beyond empagliflozin, one of Boehringer Ingelheim’s advanced development programmes taking a holistic cardio, renal and metabolic disease approach is their dual glucagon-like peptide-1 (GLP-1)/glucagon receptor (GCGR) agonist developed in partnership with Zealand Pharma. The drug advanced through to Phase II trials in adults living with obesity and also those with NASH in 2021. This programme has received FDA Fast Track designation.
“From antihypertensives to thrombolytics, anticoagulants and more, globally we have extensive research experience and our study programmes, combined with a lot of translational studies, providing us a depth of insight into cardio-metabolic diseases is informing future areas of research, with a focus on unmet need. These future areas include obesity, non-alcoholic steatohepatitis (NASH) and chronic kidney disease,” he stated.
Dr Clark concluded: “These developments bring together the disciplines that treat patients living with these comorbid diseases, helping to drive a cross-functional patient-centred approach. Being able to address these interrelated conditions via a more holistic approach is an exciting step forward and one that will hopefully make a big difference to the lives of patients living with one or more of these inter-related conditions.”
References
- Cardiovascular diseases (CVDs) [Internet]. Who.int. 2021 [cited 25 May 2022]. Available at: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
- BHF Statistics Factsheet – UK. London: British Heart Foundation; 2022. Available from: https://www.bhf.org.uk/what-we-do/our-research/heart-statistics
- Groenewegen A, Rutten F, Mosterd A, Hoes A. Epidemiology of heart failure. European Journal of Heart Failure [Internet]. 2020 [cited 30 May 2022];22(8):1342-1356.
- Human Medicines Highlights 2021 [Internet]. European Medicines Agency; 2022 [cited 8 June 2022]. Available from: https://www.ema.europa.eu/en/documents/report/…
- FDA approves Novartis Leqvio® (inclisiran), first-in-class siRNA to lower cholesterol and keep it low with two doses a year [Internet]. Novartis. 2021 [cited 8 June 2022]. Available from: https://www.novartis.com/news/media-releases/fda-approves-novartis…
- S. Food and Drug Administration Approves Camzyos™ (mavacamten) for the Treatment of Adults With Symptomatic New York Heart Association Class II-III Obstructive Hypertrophic Cardiomyopathy (HCM) to Improve Functional Capacity and Symptoms [Internet]. News.bms.com. 2022 [cited 8 June 2022]. Available from: https://news.bms.com/news/corporate-financial/2022/U.S.-Food…
- NICE recommends VAZKEPA®▼(icosapent ethyl) to reduce heart attacks and strokes in patients in England and Wales [Internet]. PharmiWeb.com. 2022 [cited 10 June 2022]. Available from: https://www.pharmiweb.com/press-release/2022-06-10/nice-recommends…
- Bristol Myers Squibb Announces Data from EXPLORER-LTE Demonstrating Sustained Improvements in Clinically Meaningful Cardiovascular Outcomes at Weeks 48 and 84 in Patients with Symptomatic Obstructive Hypertrophic Cardiomyopathy Receiving Mavacamten [Internet]. News.bms.com. 2022 [cited 10 June 2022]. Available from: https://news.bms.com/news/corporate-financial/2022/Bristol-Myers-Squibb-Announces-Data-from-EXPLORER-LTE-Demonstrating-Sustained…
- Cytokinetics Announces Data From REDWOOD-HCM OLE and GALACTIC-HF Presented as Late Breaking Science Presentations at the European Society of Cardiology Heart Failure 2022 Congress | Cytokinetics, Inc. [Internet]. Cytokinetics, Inc. 2022 [cited 10 June 2022]. Available from: https://ir.cytokinetics.com/news-releases/news-release-details/cytokinetics-announces-data-redwood-hcm…
- Positive Phase 3 study with aprocitentan demonstrates significant antihypertensive efficacy in patients with resistant hypertension [Internet]. Idorsia.com. 2022 [cited 10 June 2022]. Available from: https://www.idorsia.com/media/news-details?newsId=2758691
- MacRae C, Mercer S, Guthrie B, Henderson D. Comorbidity in chronic kidney disease: a large cross-sectional study of prevalence in Scottish primary care. British Journal of General Practice [Internet]. 2020 [cited 8 June 2022];71(704):e243-e249. Available from: https://doi.org/10.3399/bjgp20X714125
- Brück K, Jager K, Zoccali C, et al. Different rates of progression and mortality in patients with chronic kidney disease at outpatient nephrology clinics across Europe. Kidney International [Internet]. 2018 [cited 10 June 2022];93(6):1432-1441. Available from: https://doi.org/10.1016/j.kint.2018.01.008
- McGurnaghan S, Blackbourn L, Mocevic E, et al. Cardiovascular disease prevalence and risk factor prevalence in Type 2 diabetes: a contemporary analysis. Diabetic Medicine [Internet]. 2018 [cited 10 June 2022];36(6):718-725. Available from: https://doi.org/10.1111/dme.13825
- Einarson T, Acs A, Ludwig C, Panton U. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovascular Diabetology [Internet]. 2018 [cited 10 June 2022];17(1). Available from: https://doi.org/10.1186/s12933-018-0728-6
Related topics
Big Pharma, Clinical Development, Clinical Trials, Drug Development, Industry Insight, Research & Development (R&D), Therapeutics
Related organisations
Amarin Pharma Inc, Bayer, Bristol-Myers Squibb (BMS), Novartis, The European Commission (EC), The European Medicines Agency (EMA), The World Health Organization (WHO), UK Medicines and Healthcare products Regulatory Agency (MHRA), UK National Institute for Health and Care Excellence (NICE), US Food and Drug Administration (FDA)
Related drugs
Camzyos (mavacamten), Jardiance (empagliflozin), Leqvio (inclisiran), Vazkepa (icosapent ethyl), Verquvo (vericiguat)
Related people
Related diseases & conditions
cardiovascular disease (CVD), Heart attack, heart failure, heart failure with reduced ejection fraction (HFrEF), hypertrophic cardiomyopathy, Stroke, Type 2 Diabetes