Stabilising protein therapeutics with reversible PEGylation
Posted: 27 January 2022 | Hannah Balfour (European Pharmaceutical Review) | No comments yet
Researchers demonstrate the efficacy and safety of stabilising protein drugs with a reversible PEGylation material called PEG-PRX.
Japanese researchers have developed a new material that binds to protein drugs, prolonging their duration of their effect without impairing their activity, thereby improving overall drug performance.
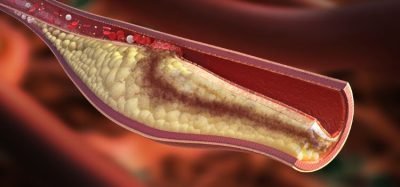
Recombinant protein therapeutics have gained significant attention over the past decade, with many being approved for the treatment of conditions ranging from cancer to infections to genetic abnormalities. Yet, these drugs often have limited stability under physical stress, which can impair their bioactivity, and are quickly eliminated from the bloodstream, limiting the duration of their effect and efficacy.
To overcome these challenges, scientists devised a method of adding polyethylene glycol (PEG, a polymer produced from petroleum) to proteins, to extend the drug’s sustainability in blood and prevent clumping. Unfortunately, tight binding of PEG chains interferes with the proteins, resulting in reduced or complete loss of drug activity. This problem fostered research on the development of removable and reversible PEGylation materials that could be added and removed as and when required.
In this vein, Associate Professor Taishi Higashi and his team of researchers at Kumamoto University, Japan, published their new study in Materials Today Bio. The research used the compound polyrotaxane (PRX) to create a new “supramolecular” material that could reversibly add PEG chains to proteins without impairing their activity. First, they created a reversible agent called PEG-PRX by mixing PEG with PRX, and then coupled it with insulin to form the PEG-PRX-Insulin complex. When administered to diabetic rats, the complex maintained the effect of insulin without compromising its activity.
Based on previous work with another PEGylation material created using cyclodextrin, unsuccessful due to a mismatch in shapes and charge distributions resulting in the binder being easily removed, the team developed this new PEG agent to deform according to the shape and charge of the protein. Dr Higashi explained: “When the PRX molecule with a positive charge is mixed with a protein with a negative charge such as insulin, the complex becomes both flexible and efficient. This flexibility appears to be critical for the efficient assembly of complexes.”
To ascertain the material’s flexibility, the authors compared their PRX derived experimental outcomes to those of a less flexible agent, dextran (DEX). In the comparisons, it was clear that the PRX interactions were much stronger and kept the insulin more tightly bound in the complex, increasing both the stability and availability of the drug.
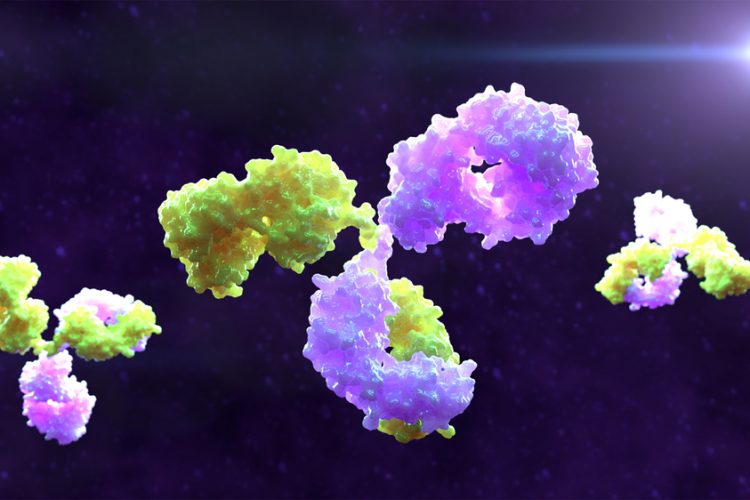
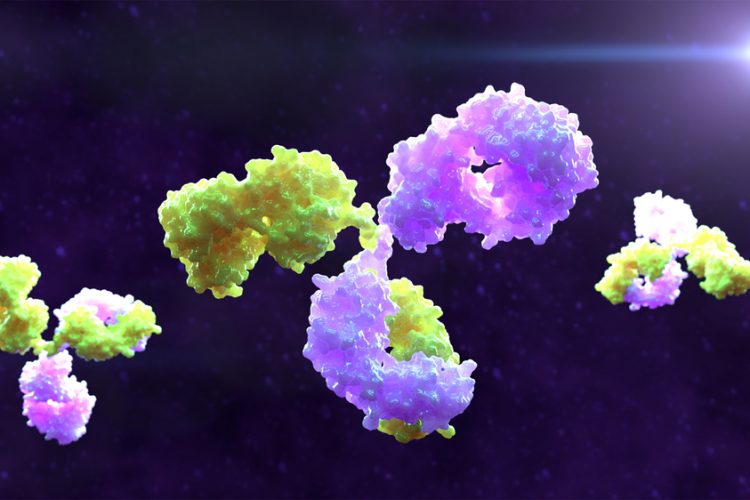
Based on these findings, the researchers began work with antibodies, which have gained popularity as first-line treatment modalities for different cancer types but are impacted by aggregation during transportation and storage. Aggregation leads to the loss of antibody activity resulting in serious side effects. By conducting shaking stress experiments, the authors confirmed that adding the novel PEG-PRX agent to antibodies resulted in no aggregate formation after seven days, whereas 90 percent of the antibodies in the control group aggregated. “We obtained excellent results not just with the standard but also with a commercial antibody drug, suggesting that our material has great potential to be a stabilising agent for these medicinal agents,” enthused Dr Higashi.
He concluded: “Because this supramolecular material can ameliorate the flaws of diverse protein drugs simply by mixing them together, we expect it will be used as a pharmaceutical material with both efficacy and flexibility.”
Related topics
Antibodies, Biologics, Drug Development, Drug Safety, Formulation, Ingredients, protein structure, Proteins, Research & Development (R&D), Therapeutics