“Universal” CRISPR-edited T cells improve resistant leukaemia
Posted: 2 November 2022 | Catherine Eckford (European Pharmaceutical Review) | No comments yet
Children with leukaemia were successfully treated with first-in-human “universal” CRISPR-edited T-cells, by researchers at Great Ormond Street Hospital and University College London.
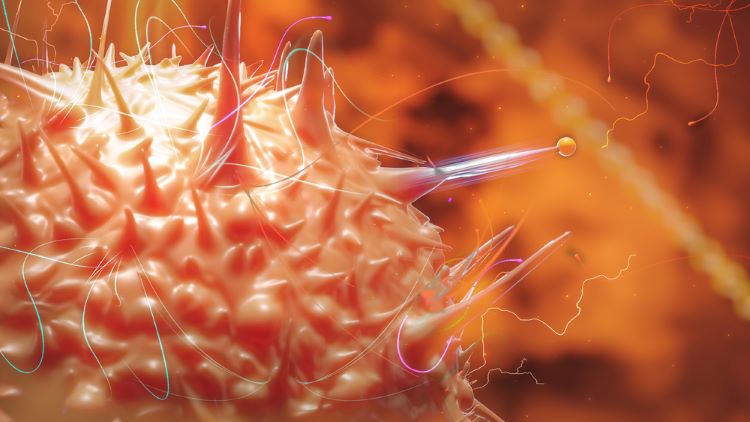
Researchers at Great Ormond Street Hospital for Children (GOSH) and University College London (UCL) Great Ormond Street Institute of Child Health (UCL GOS ICH) have used “universal” CRISPR-edited cells in humans for the first time to treat B-cell acute lymphoblastic leukaemia (B-ALL) child patients with engineered donor T cells. The treatment did not require matching donor cells, a major step in developing gene-edited cells for cancer treatment.
The Phase I trial, published in Science Translational Medicine, involved building and applying a new generation of universal genome-edited T cells, a better solution to current chimeric antigen receptors (CAR) T-cell therapies which rely on collecting and engineering a patient’s own cells, an expensive and lengthy process.
To modify the T cells, CRISPR technology cut into and inserted a genetic code into the cells’ DNA, enabling the T cells to express a CAR, which recognises a marker on the surface of cancerous B cells and destroys them.
Researchers manufactured banks of donor CAR T-cells using one disabled virus. This helped to transfer the CAR and the CRISPR guidance systems. mRNA technology was then applied to activate the gene editing steps.
The CRISPR clinical trial
The trial involved six children aged 14 months to 11 years with relapsed and treatment-resistant leukaemia. Four out of the first six children entered remission in 28 days, making them eligible for stem cell transplant. Two participants continue to be in remission nine and 18 months post-treatment respectively. Two children relapsed after receiving the stem cell transplant.
The side effects observed in the study were expected by researchers. One patient required intensive care for a short period.
Dr Kanchan Rao, Consultant in Bone Marrow Transplant at GOSH explained: “This study adds to the growing body of evidence that genome-edited T cells can be a viable alternative to currently available treatments.”
Researchers plan to offer earlier treatment to a larger patient population.
The following organisations funded the research:
- National Institute of Health and Care Research (NIRH)
- NIHR GOSH Biomedical Research Centre
- Medical Research Council (MRC).
Related topics
Related organisations
Great Ormond Street Hospital (GOSH), University College London (UCL)









