Microbiome therapeutic development boosted by metabolomics
Posted: 15 February 2021 | Christopher Ford (Seres Therapeutics) | No comments yet
There is a growing adoption of metabolomics to support drug discovery and development. Metabolomics involves the comprehensive analysis of metabolites in biological specimens. As such, it is commonly used for the discovery and validation of biomarkers that can support critical decisions in the drug development process. In this article, Christopher Ford, Senior Director at Seres Therapeutics, recounts how metabolomic data supported a Phase III trial redesign, aiding further development of a novel microbiome therapeutic investigational drug candidate for the company.
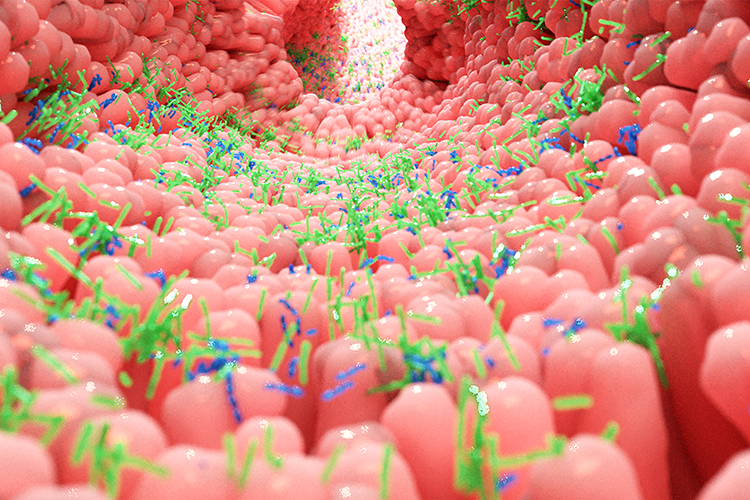
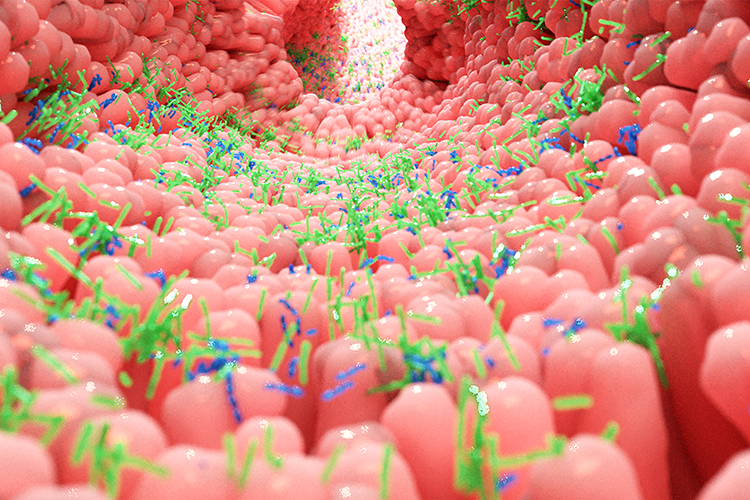
THE HUMAN microbiome describes the full array of microorganisms that live on and in humans. Most of these microbes supply crucial ecosystem services that benefit the entire host-microbe system and studies have shown that disruption of the human microbiome, either through loss of beneficial functions or the introduction of maladaptive functions by invading microbes, can contribute to disease.1 While the collection of microbial genomes, or metagenome, can provide information relating to the diversity of these microbes, it is not sufficient to detail the function of the microbiome. The unique capability of metabolomics to measure microbiome-derived metabolites sheds light on the biological activity of bacterial communities in ways that other omics technologies cannot.
Seres Therapeutics, a late clinical-stage biotechnology company, is developing novel microbiome therapeutic investigational drug candidates for a wide range of diseases, that work by modulating the function of the human intestinal microbiome. “The concept underpinning our therapeutics is that our bodies are in constant crosstalk with bacterial communities, critical for maintaining a state of health,” said Christopher Ford, Senior Director, Computational Microbiome Sciences at Seres Therapeutics. He explained that the company is particularly interested in understanding the function of the microbial community in the healthy gut. “The gastrointestinal (GI) system is heavily built up of immune cells that sit in and around that GI tissue. The bacterial community in your gut has a direct interaction with your immune system and is key part of the way in which your body establishes immune homeostasis.
“For example, there is a lot of emerging data in the immuno-oncology field that supports the concept that the body’s ability to respond to a new type of cancer therapeutic, called immune checkpoint inhibitors, is in part dependent on the gut microbes that are present in your GI system,” he explained. “It is an incredibly complex science to not only understand that interaction, but to then try to modulate it.”
In their effort to develop effective investigational microbiome therapeutics, researchers at Seres are harnessing the power of metabolomics to understand the function of the gut bacteria. In contrast to conventional therapeutics, which target just one disease pathway, bacterial consortia are multifunctional, meaning they can have multiple pharmacological effects and modulate numerous functional pathways within the body to achieve therapeutic impact. Over the past decade, the company has pioneered the translation of microbiome insights into what may become an entirely new class of medicines, two of which are in late-stage clinical testing. Current late stage programmes include therapeutics targeting Clostridioides difficile, formerly known as Clostridium difficile and ulcerative colitis.
Unmet clinical need
C. difficile is a healthcare-associated infection and significant source of potentially preventable morbidity and death, particularly among hospitalised older adults. The current standard of care for C. difficile infection is antibiotics; however, antibiotic treatment alone is ineffective against dormant spore forms of C. difficile, which can germinate and grow after antibiotics are completed, leading to a vicious cycle of recurrence. Repeated antibiotic exposure also depletes beneficial bacteria that inhibit C. difficile, increasing the risk of recurrence.
Development pathway
Ford explained that an abundance of literature, both experimental and observational studies, have demonstrated that the microbiome plays a major role in C. difficile recurrence. “We knew that breaking this cycle of recurrence would require a novel microbiome therapeutic.” To address this, Seres is developing SER‑109 – an investigational, oral, biologically-derived microbiome therapeutic designed to prevent C. difficile recurrence.2 SER-109 is a consortium of purified bacterial spores of multiple Firmicute species, manufactured by fractionating targeted bacteria from stool of screened and tested healthy human donors with further steps to inactivate and remove most potential pathogens.3,4
Following the initial development stages, the researchers used standard genomic methods to further understand how their therapy was working. “We had to start making decisions about how often to dose, when to dose and how much dose to give. We also looked at the changes that were being catalysed to understand whether we were seeing the clinical outcome we wanted and how this related back to the function of our therapy,” said Ford.
Following a successful Phase I study, SER-109 advanced into Phase II. “We were disappointed to find that we got a non-significant clinical outcome between placebo and SER-109 in the Phase II study given the prior study results,” said Ford. To address this unexpected hurdle, the team leveraged global metabolomics to discover biomarkers and targeted metabolomics5 of the bile acids to validate their data in compliance with regulatory standards. The reproducibility and high quality of the data increased the confidence in how their microbiome therapeutic was changing the metabolism of particular bile acids in the GI system, which relate directly to the pathogenesis of C. difficile. “From these data, we saw that the change in bile acids in our Phase II study was suboptimal relative to what we had achieved in Phase I,” said Ford.
The resultant metabolomic data in combination with other microbiome data allowed Seres to have a much clearer picture of the biological activity of the microbial community and to identify potential metabolite-based biomarkers that could inform drug pharmacokinetics and pharmacodynamics. Insights such as these from the Phase I and II, informed the design of the company’s Phase III study. “We are now coming off of a highly successful Phase III study, designed in part based on those data,” said Ford. “It was a pivotal moment in troubleshooting that trial and moving the product forward. The use of global metabolomics to help us evaluate drug activity in the Phase I and Phase II, and to then inform a successful Phase III was particularly valuable.”
Quality data
Ford highlighted the importance of quality data and data validation in these trials, especially when dealing with the regulators. “We are working in a completely novel space; there is value in not just defining efficacy and safety, but also the mechanism of our drugs. Having quality data that is both well-documented and also reproducible and rigorous, is very valuable in a regulatory setting. We need to be able to stand behind these data because it is what will allow us to engage with experts and clinicians.”
Ford concluded: “Seres has endeavoured to build a cross-functional, differentiated, reverse translational platform that would enable us to not only put drugs forward, but also to understand how they work to both support the development of those therapies and to inform the development of new therapies in the space. Seres has high quality, placebo-controlled data from multiple clinical assets that we can use to refine our knowledge about which bacterial species, functions and metabolites are associated with or driving health outcomes. We can then use that to drive the next wave of therapies, whether that be for novel diseases or for a modified approach to diseases we are already working in.”
About the author
Christopher Ford, PhD is the Senior Director of Computational Microbiome Sciences at Seres Therapeutics. He has over 14 years of combined research experience in microbial genomics, bioinformatics, and bacterial pathogenesis. At Seres, he has been involved in the discovery and development of multiple microbiome therapeutics, including key roles on SER-109, SER-155, and SER-301.
References
- Young V. The role of the microbiome in human health and disease: an introduction for clinicians. BMJ. 2017;j831.
- Our Programs [Internet]. Seres Therapeutics. 2021 [cited 2 February 2021]. Available from: https://www.serestherapeutics.com/ourprograms/
- Khanna et al. A Novel Microbiome Therapeutic Increases Gut Microbial Diversity and Prevents Recurrent Clostridium difficile Infection. JID, 2016;jiv766
- McGovern, Ford, Henn et al. SER-109, an Investigational Microbiome Drug to Reduce Recurrence after Costridioides difficile infection: Lessons Learn from a Phase 2 Trial. CID, 2020;ciaa387
- Metabolon – Enlightening Life [Internet]. Metabolon. 2021 [cited 2 February 2021]. Available from: https://www.metabolon.com/
Issue
Related topics
Clinical Development, Clinical Trials, Drug Development, Drug Safety, Microbiomes, Research & Development (R&D), Therapeutics
Related organisations
Related drugs
Related diseases & conditions
C. Difficile, Clostridioides difficile, Clostridium Difficile









